5.3 Case Study: Celiac Disease
Hannah Nelson and Christelle Sabatier
Learning Objectives
- Describe the impact of surface area on nutrient absorption.
- Apply knowledge of celiac disease to identify foods to avoid for those with celiac disease.
Understanding Celiac Disease, Diagnosis, Complications, and Approach to Treatment
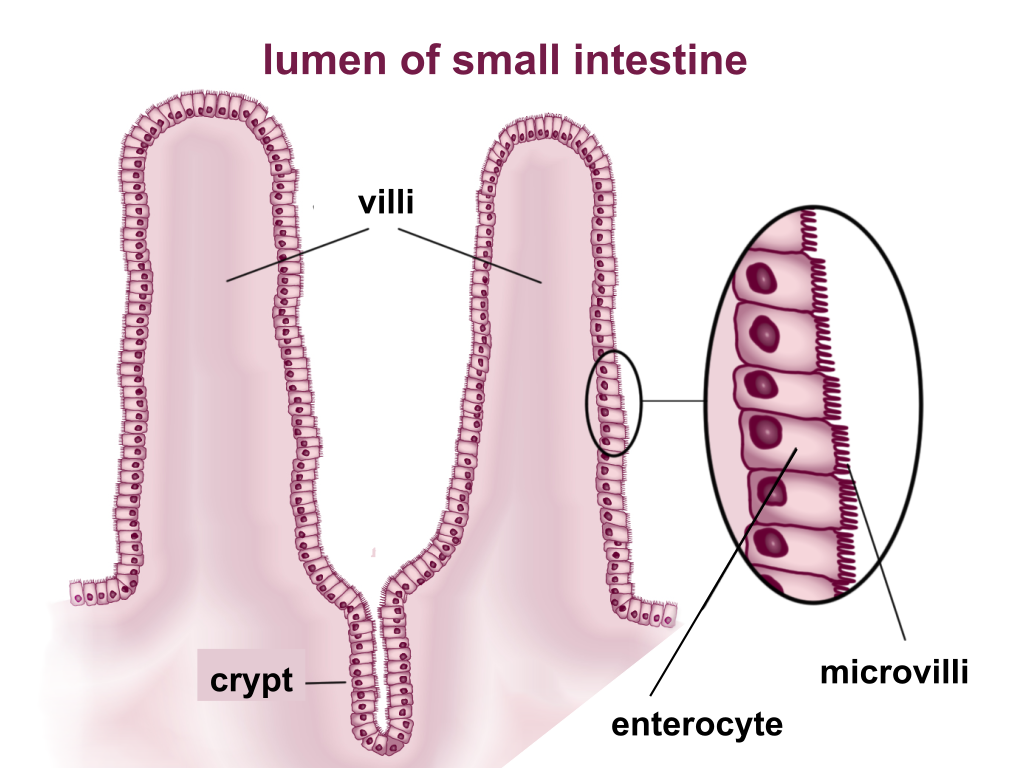
The human digestive tract from the ingestion to excretion is approximately 30 feet, varying slightly by the size of each individual. The series of digestive organs involved in digestion require substantial length in order to provide sufficient time and surface area for breakdown and absorption of material. Within the small and large intestines, surface area is the most crucial. The small intestine is studded with villi, small hairlike projections off of the intestinal lumen. These villi are composed of a central core with a muscle strand, vein, and centrally located artery. The individual epithelial cells on the surface of the villi that contact the intestinal lumen are covered in more hairlike projections, called microvilli. These projections increase surface area for nutrient absorption in the small intestine. There are no villi or microvilli present in the large intestine. The large intestine absorbs electrolytes, water, and essential vitamins.
The inadequate absorption of nutrients from the gut, malabsorption, leads to increased likelihood for disease and cardiac issues. Malabsorption of micro- and macronutrients can be caused by a variety of issues, including autoimmune disorders, pancreatic insufficiency, parasitic infections, and alcohol abuse.
Autoimmune disorders are a class of medical conditions which cause the immune system to inappropriately attack parts of the body. Celiac disease is an autoimmune disorder that results in an inability to eat gluten (a protein component of wheat) due to an intolerance for the molecule in the digestive tract, where it can cause irreversible damage. Individuals with Celiac disease have an immune response to gluten, which results in damage to the small intestine villi. There is no cure for celiac disease, but it is treated by a gluten-free diet (often supervised by a dietician). In cases where patients present with all accompanying symptoms and have undergone genetic testing, celiac disease can be diagnosed without any procedures.
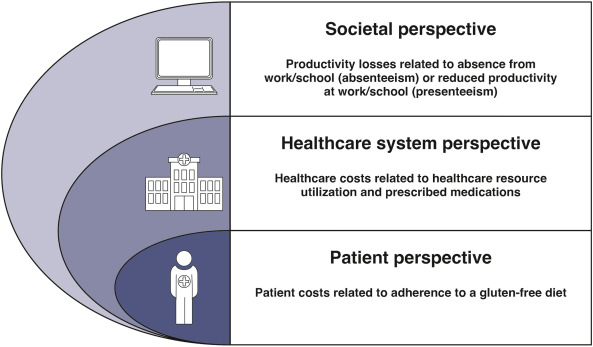
Celiac disease itself is not deadly; however, the consequences of symptoms can be. Malnourishment, chronic anemia, and increased risk of certain cancers can ultimately lead to a fatal outcome. Celiac is thought to be an incredibly underdiagnosed condition, theoretically only diagnosed in 25% of the population that it should. In populations where the dominant culture consumes more gluten, the symptomatology is made more obvious. Some populations have higher incidences of gluten intolerance. For example, Finland and Algeria have two of the highest rates of country-wide celiac disease diagnosis. Undiagnosed individuals struggle with manage daily tasks resulting in reduced productivity (Figure 5.3.2) which presents a significant economic burden.
Traditionally, the autoimmune disorder’s complicated symptoms require a complicated and expensive diagnostic effort. Using labs, history, and an endoscopic biopsy, an assessment can be made with great accuracy. Celiac disease once diagnosed is assessed with a Marsh Score, a system created by Dr. Michael Marsh.
Healthcare providers may refer to celiac disease as “mild” in patients with grade 1 or 2 intestinal damage. This can be misleading because the severity of damage does not determine the presence or overall severity of celiac disease. An individual either has celiac disease or does not, regardless of the extent of intestinal damage.
The diagnosis of this autoimmune disorder is in many ways an ethical concern for doctors and scientific professionals. While an endoscopic biopsy is the most successful diagnostic tool, these tests are difficult to plan, painful, and incredibly expensive. For those without health insurance, testing via this method can essentially be an impossibility. Doctors must use other ways of diagnosis, and an overly cautious attitude in such cases. Black (63%) and Hispanic (49%) Americans are more likely to have no awareness of their own celiac disease or gluten sensitivity, compared with White Americans (47%), suggesting a large potential health inequity in treatment and diagnosis of the disease.
Avoiding gluten can be tricky and expensive. The usual suspects that contain gluten are wheat, barley, bulgur, durum, farina, graham flour, malt, rye, semolina, spelt (wheat form), and triticale. However, gluten can also be hidden in other products, such as soy sauce, modified food starch, preservatives, over the counter medications, vitamins and supplements, lipstick and other makeup products, toothpaste, mouthwash, communion wafers, and even envelope stamp glue.
Celiac disease can easily be confused or conflated with gluten intolerance. This is an inflammatory reaction in the small intestine, as it cannot fully absorb gluten molecules. Individuals with this problem similarly remove gluten from their diet.
Practice Questions
References
Beyond Celiac. (n.d.). Celiac disease and health equity. Retrieved August 2, 2025, from https://www.beyondceliac.org/celiac-disease-and-health-equity/.
Bozorg, S. R., Lee, A. R., Mårild, K., & Murray, J. A. 2024. “The economic iceberg of celiac disease: more than the cost of gluten-free food.” Gastroenterology, 167(1):172–82.
Figure Descriptions
Figure 5.3.1. The image is an anatomical illustration depicting sections of the small intestine. It shows two main projections labeled as “villi” that extend into the lumen of the small intestine. Each villus is lined with small cell-like structures. Below the villi, a depression labeled as “crypt” is visible, indicating the small gaps between the villi. An enlarged circular inset on the right side of the image provides a close-up view of the intestinal lining, showing the structure of cells called “enterocytes” with protrusions labeled as “microvilli.” The microvilli appear as fine, hair-like extensions on the surface of enterocytes. The illustration is predominantly in shades of pink and red. [Return to Figure 5.3.1]
Figure 5.3.2. The image is a diagram illustrating three perspectives related to costs and impacts, arranged in overlapping semicircular layers. Starting from the outermost layer, the “Societal perspective” is represented by a computer icon and includes information about productivity losses due to absenteeism and presenteeism. Below, the “Healthcare system perspective” is depicted with a hospital icon and focuses on healthcare costs related to resource utilization and medications. The innermost layer is the “Patient perspective,” shown with a human figure icon, detailing costs related to adhering to a gluten-free diet. Each section has corresponding text explaining the particular perspective. [Return to Figure 5.3.2]
Media Attributions
- Villi_&_microvilli_of_small_intestine.svg © BallenaBlanca is licensed under a CC BY (Attribution) license
- CeD economic burden © Bozorg, Lee, Marild, and Murray is licensed under a CC BY (Attribution) license
