21.2 How Hormones Regulate Blood Glucose Levels
Learning Objectives
By the end of this section, you will be able to do the following:
- Describe the role of glucagon in regulating blood glucose levels.
- Describe the role of insulin in regulating blood glucose levels.
- Explain the impact of insulin deficiency on blood glucose homeostasis.
Blood glucose levels vary widely over the course of a day as periods of food consumption alternate with periods of fasting. Insulin and glucagon are the two hormones primarily responsible for maintaining homeostasis of blood glucose levels. Additional regulation is mediated by the thyroid hormones.
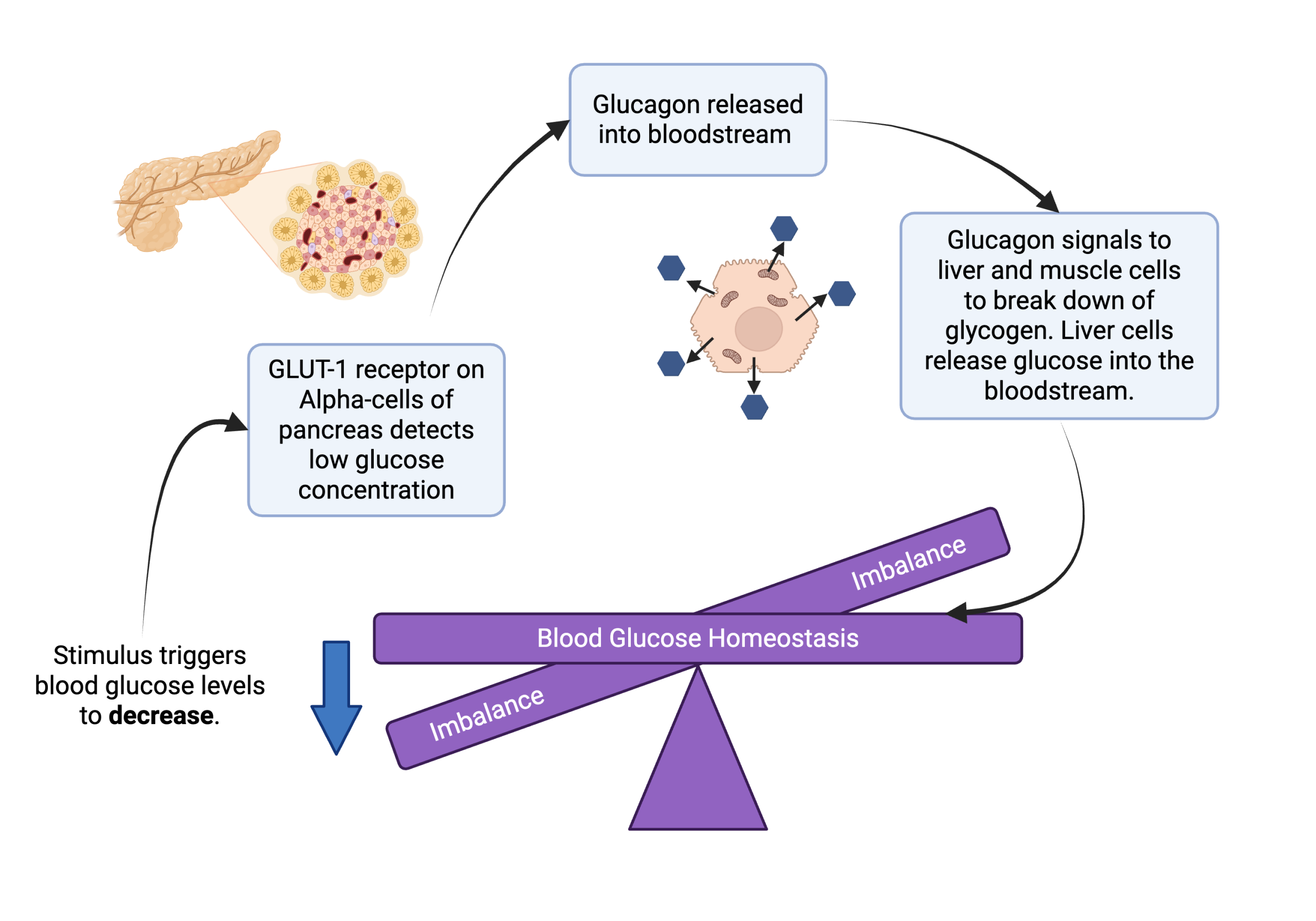
Regulation of Blood Glucose Levels by Glucagon
When blood glucose levels decline below normal levels, for example between meals or when glucose is utilized rapidly during exercise, the hormone glucagon is released from the alpha cells of the pancreas. Glucagon raises blood glucose levels, eliciting what is called a hyperglycemic effect, by stimulating the breakdown of glycogen to glucose in skeletal muscle cells and liver cells in a process called glycogenolysis. Glucose can then be utilized as energy by muscle cells and released into circulation by the liver cells (Figure 21.2.1). Glucagon also stimulates absorption of amino acids from the blood by the liver, which then converts them to glucose. This process of glucose synthesis is called gluconeogenesis. Glucagon also stimulates adipose cells to release fatty acids into the blood. These actions mediated by glucagon result in an increase in blood glucose levels to normal homeostatic levels. Rising blood glucose levels inhibit further glucagon release by the pancreas via a negative feedback mechanism.
Regulation of Blood Glucose Levels by Insulin
Cells of the body require nutrients in order to function, and these nutrients are obtained through feeding. In order to manage nutrient intake, storing excess intake and utilizing reserves when necessary, the body uses hormones to moderate energy stores. Insulin is produced by the beta cells of the pancreas, which are stimulated to release insulin as blood glucose levels rise (for example, after a meal is consumed). Insulin lowers blood glucose levels by enhancing the rate of glucose uptake and utilization by target cells such as liver cells and skeletal muscle cells, which have the capacity to store carbohydrates. Specifically, it stimulates liver and skeletal muscle cells to convert glucose to glycogen, which is then stored by cells for later use. Insulin also increases glucose transport into certain cells. This results from an insulin-mediated increase in the number of glucose transporter proteins in cell membranes, which remove glucose from circulation by facilitated diffusion (Figure 21.2.2).
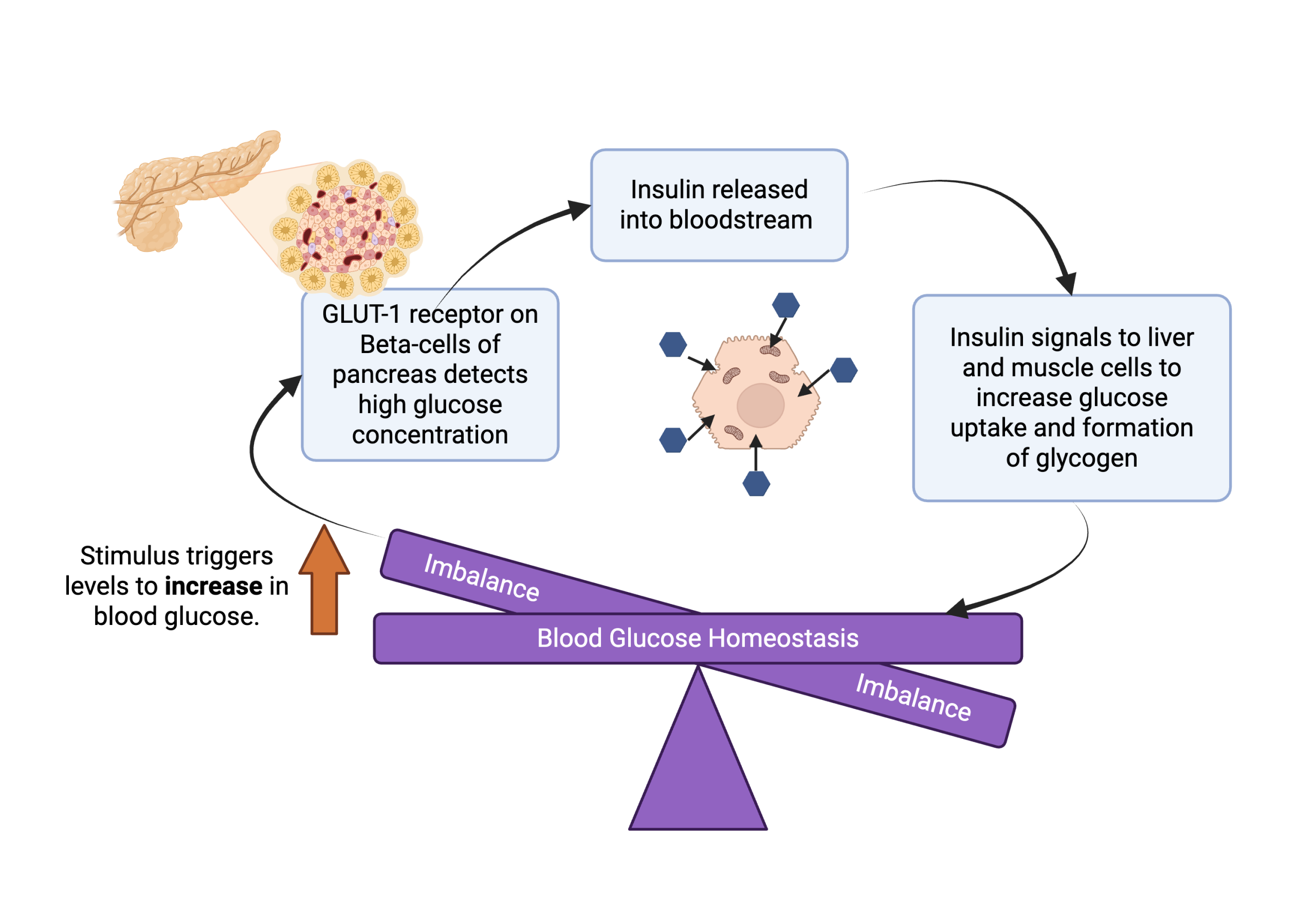
As insulin binds to its target cell via insulin receptors and signal transduction, it triggers the cell to incorporate glucose transport proteins (GLUT-4) into its membrane. This allows glucose to enter the cell, where it can be used as an energy source. However, this does not occur in all cells: some cells, including those in the kidneys and brain, can access glucose without the use of insulin. Insulin also stimulates the conversion of glucose to fat in adipocytes and the synthesis of proteins. These actions mediated by insulin cause blood glucose concentrations to fall, called a hypoglycemic “low sugar” effect, which inhibits further insulin release from beta cells through a negative feedback loop.
Video 21.2.1. Understanding Type 2 Diabetes by Animated Diabetes Patient
Impaired insulin function can lead to a condition called diabetes mellitus, which is characterized by unusually high blood glucose levels (hyperglycemia). If left untreated, this can be dangerous and cause vision loss, strokes, and lethargy. This can be caused by low levels of insulin production by the beta cells of the pancreas (type 1 diabetes), or by reduced sensitivity of tissue cells to insulin (type 2 diabetes). In both cases, this prevents glucose from being absorbed by cells, causing high blood glucose levels, or hyperglycemia (high sugar). High blood glucose levels make it difficult for the kidneys to recover all the glucose from nascent urine, resulting in glucose being lost in urine. High glucose levels also result in less water being reabsorbed by the kidneys, causing high amounts of urine to be produced; this may result in dehydration. Over time, high blood glucose levels can cause nerve damage to the eyes and peripheral body tissues, as well as damage to the kidneys and cardiovascular system. Oversecretion of insulin can cause low blood glucose levels, or hypoglycemia (low sugar). This causes insufficient glucose availability to cells, often leading to muscle weakness and sometimes even to unconsciousness or death if left untreated.
Practice Questions
Glossary
diabetes mellitus
A chronic condition caused by impaired insulin signaling and characterized by unusually high blood glucose levels if left untreated.
type I diabetes
A form of diabetes mellitus caused by low levels of insulin production by the beta cells of the pancreas.
type II diabetes
A form of diabetes mellitus caused by a reduced sensitivity of tissue cells to insulin.
Figure Descriptions
Figure 21.2.1. The diagram illustrates the process of blood glucose homeostasis, focusing on the role of glucagon. At the top left, an image of the pancreas is shown with highlighted alpha-cells. Below it, there’s an arrow pointing to a box stating, “GLUT-1 receptor on Alpha-cells of pancreas detects low glucose concentration.” This connects to another box stating “Glucagon released into bloodstream,” leading to a cellular depiction. Arrows connect to another box that reads, “Glucagon signals to liver and muscle cells to break down glycogen. Liver cells release glucose into the bloodstream.” Below, a balance labeled “Blood Glucose Homeostasis” is tilted, with an arrow indicating a decrease in blood glucose levels, marked by the term “Imbalance” on each side. [Return to Figure 21.2.1]
Figure 21.2.2. The image is an illustrative flowchart depicting the role of insulin in blood glucose homeostasis. In the top left corner, a detailed view of the pancreas highlights the beta-cells with GLUT-1 receptors detecting high glucose concentration. Arrows indicate the process, starting from the detection of high glucose, leading to insulin release into the bloodstream. The flow continues to depict how insulin signals the liver and muscle cells to increase glucose uptake and form glycogen. At the bottom, a seesaw labeled “Blood Glucose Homeostasis” indicates balance, with the word “Imbalance” on both tilting sides. An upwards arrow labeled “Stimulus triggers levels to increase in blood glucose” points to the starting point of the process. [Return to Figure 21.2.2]
Media Attributions
- 1C_Homeostasis – Glucagon © BioRender adapted by Christelle Sabatier is licensed under a CC BY-NC (Attribution NonCommercial) license
- 1C_Homeostasis – Insulin © BioRender adapted by Christelle Sabatier is licensed under a CC BY-NC (Attribution NonCommercial) license
