Chapter 12. The Respiratory System
12.1 Organs and Structures of the Respiratory System
Learning Objectives
By the end of this section, you will be able to:
- describe the major functions of the respiratory system;
- describe and diagram the anatomy of and branching structure of the respiratory airways, starting at the trachea and ending at the alveoli;
- describe the locations of and importance of ciliated epithelium in the respiratory tract; and
- compare and contrast the functions of type I and type II alveolar cells.
The respiratory system functions primarily to:
- provide oxygen to body tissues for cellular respiration;
- eliminate the carbon dioxide produced in metabolism; and
- help to maintain acid-base balance. Acid-base balance is discussed in Chapter 14.
In addition, portions of the respiratory system are used for olfaction, for speech production, and for straining during events such as during childbirth or coughing.
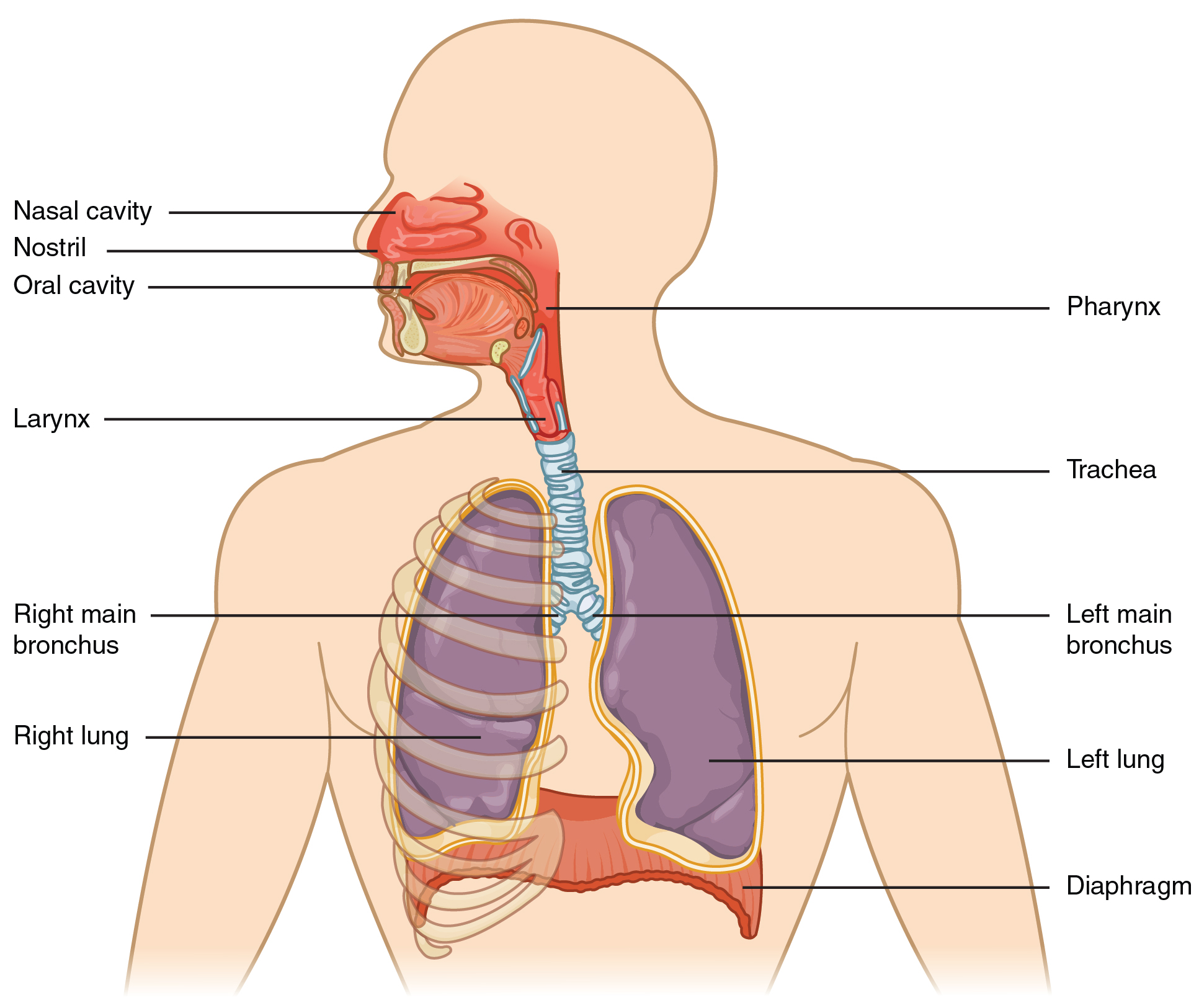
Functionally, the respiratory system can be divided into a conducting zone and a respiratory zone. The conducting zone of the respiratory system includes the organs and structures not directly involved in gas exchange: the nose and nasal cavities, the pharynx, the larynx, the trachea, the bronchi, and most of the bronchial tree. As no gas exchange takes place here, these airways constitute the anatomical dead space and have a volume of approximately 150 mL.
Gas exchange occurs in the respiratory zone. The lungs house some portions of the conducting zone and all of the respiratory zone. The lungs are discussed in detail in Section 12.2.
Conducting Zone Structures
The major functions of the conducting zone are to provide a route for incoming and outgoing air, to remove debris and pathogens from the incoming air, and to warm and humidify the incoming air. Several structures within the conducting zone perform other functions as well. The epithelium of the nasal passages, for example, is essential in olfaction (smell), and the bronchial epithelium that lines the lungs can metabolize some airborne carcinogens.
The Nose and Nasal Cavity
The major entrance and exit for the respiratory system is the nose. When discussing the nose, it is helpful to divide it into two major sections: the external nose and the nasal cavity.
The external nose consists of the surface and skeletal structures that result in the outward appearance of the nose and contribute to its numerous functions. The nares, or nostrils, open into the nasal cavity, which is separated into left and right sections by the nasal septum (Figure 12.1.1 and Figure 12.1.2).
Each lateral wall of the nasal cavity has three mucosa-lined nasal conchae. Conchae project into the nasal cavity; grooves inferior to the conchae are called meatuses. Conchae serve to increase the surface area of the nasal cavity and to disrupt the flow of air as it enters the nose, causing air to bounce along the epithelium, where it is cleaned and warmed. The conchae and meatuses also conserve water and prevent dehydration of the nasal epithelium by trapping water during exhalation.
The floor of the nasal cavity is composed of the palate. The hard palate at the anterior region of the nasal cavity is composed of bone. The soft palate at the posterior portion of the nasal cavity consists of muscle tissue. Air exits the nasal cavities via the internal nares and moves into the pharynx.
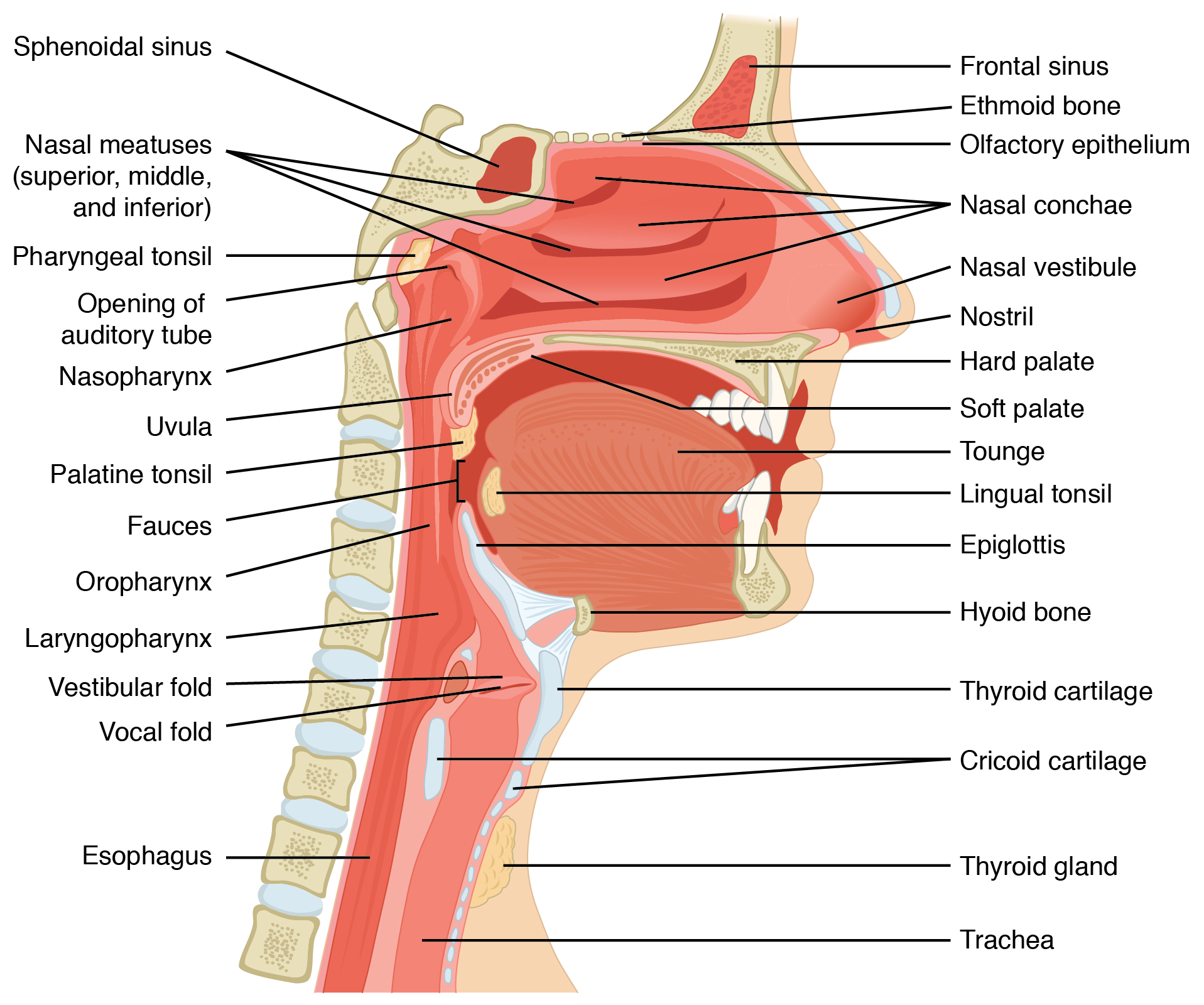
Several bones that help form the walls of the nasal cavity have air-containing spaces called the paranasal sinuses, which serve to warm and humidify incoming air. Sinuses are lined with a mucosa. Each paranasal sinus is named for its associated bone: frontal sinus, maxillary sinus, sphenoidal sinus, and ethmoidal sinus. The sinuses produce mucus and lighten the weight of the skull.
The nares and anterior portion of the nasal cavities are lined with mucous membranes, containing sebaceous glands and hair follicles that serve to prevent the passage of large debris, such as dirt, through the nasal cavity. An olfactory epithelium that detects odors is found deeper in the nasal cavity.
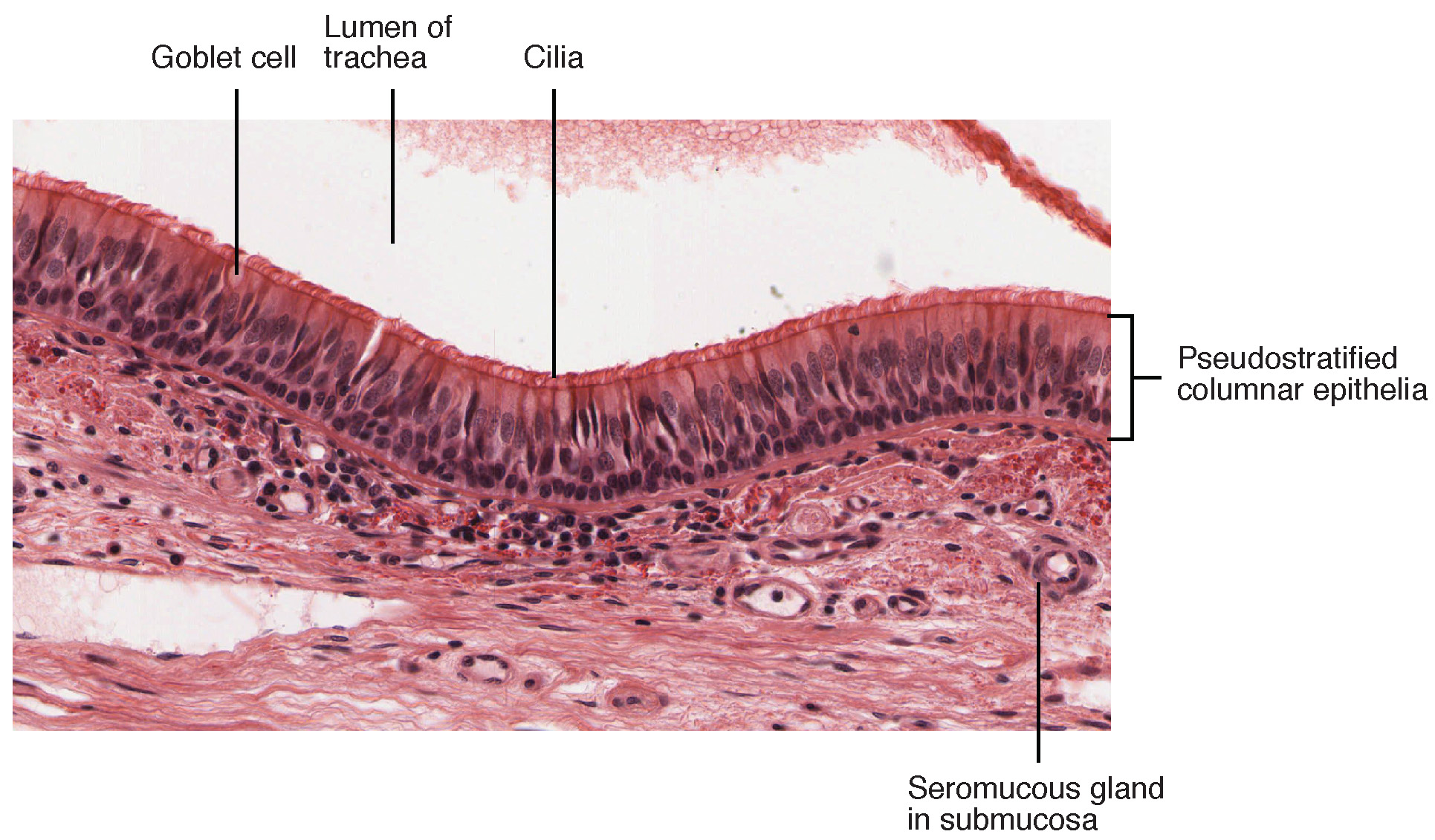
The conchae, meatuses, and paranasal sinuses are lined by respiratory epithelium composed of pseudostratified ciliated columnar epithelium (Figure 12.1.3). This epithelium contains goblet cells, one of the specialized, columnar epithelial cells that produce mucus to trap debris. The cilia of the respiratory epithelium help remove the mucus and debris from the nasal cavity with a constant beating motion, sweeping materials towards the throat to be swallowed. This moist epithelium functions to warm and humidify incoming air: capillaries located just beneath the nasal epithelium warm the air by convection. Serous and mucus-producing cells also secrete an enzyme called lysozyme and proteins called defensins, both of which have antibacterial properties. Immune cells that patrol the connective tissue deep to the respiratory epithelium provide additional protection.
Cold air slows the movement of the cilia, resulting in accumulation of mucus that may in turn lead to a runny nose during cold weather.
Pharynx
The pharynx is a tube formed by skeletal muscle and lined by a mucosa (mucous membrane) that is continuous with that of the nasal cavities (Figure 12.1.2). The pharynx is divided into three major regions: the nasopharynx, the oropharynx, and the laryngopharynx (Figure 12.1.4).
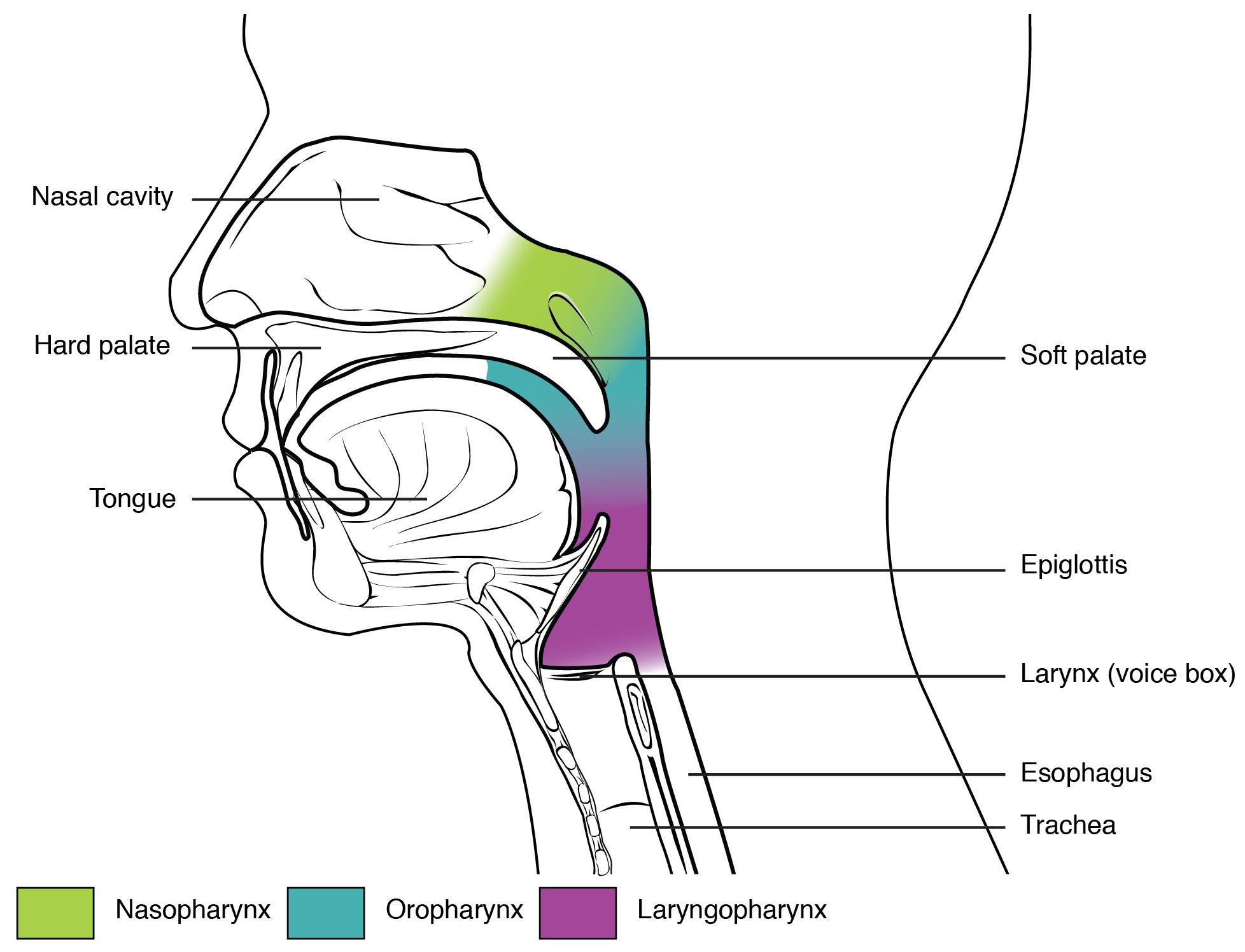
The nasopharynx is flanked by the conchae of the nasal cavity, and it serves only as an airway. At the top of the nasopharynx are the pharyngeal tonsils. A pharyngeal tonsil is an aggregate of lymphoid reticular tissue that lies at the superior portion of the nasopharynx (Figure 12.1.2). The function of the pharyngeal tonsil is not well understood, but it contains a rich supply of lymphocytes and is covered with ciliated epithelium that traps and destroys invading pathogens that enter during inhalation. The pharyngeal tonsils are large in children, but interestingly, tend to regress with age and may even disappear.
The uvula is a small bulbous, teardrop-shaped structure located at the apex of the soft palate. Both the uvula and soft palate move like a pendulum during swallowing, swinging upward to close off the nasopharynx to prevent ingested materials from entering the nasal cavity.
Auditory (Eustachian) tubes that connect to each middle ear cavity open into the nasopharynx. These tubes are closed except when yawning or swallowing. The functions of the auditory tubes are to equalize pressure between the middle ear and the environment, to drain fluid from your middle ear, and to protect your middle ear from viruses and bacteria.
The oropharynx is a passageway for both air and food. The oropharynx is bordered superiorly by the nasopharynx and anteriorly by the oral cavity. As the nasopharynx becomes the oropharynx, the epithelium changes from pseudostratified ciliated columnar epithelium to stratified squamous epithelium. The oropharynx contains two distinct sets of tonsils, the palatine and lingual tonsils. A palatine tonsil is one of a pair of structures located laterally in the oropharynx in the area of the fauces. The lingual tonsil is located at the base of the tongue. Similar to the pharyngeal tonsil, the palatine and lingual tonsils are composed of lymphoid tissue, and they trap and destroy pathogens entering the body through the oral or nasal cavities.
The laryngopharynx is inferior to the oropharynx and posterior to the larynx. It continues the route for ingested material and air until its inferior end, where the digestive and respiratory systems diverge. The stratified squamous epithelium of the oropharynx is continuous with the laryngopharynx. Anteriorly, the laryngopharynx opens into the larynx, whereas posteriorly, it enters the esophagus.
Larynx
The larynx is a cartilaginous structure inferior to the pharynx that connects the pharynx to the trachea (Figure 12.1.5). The structure of the larynx is formed by several pieces of cartilage. Three large cartilage pieces—the thyroid cartilage (anterior), epiglottis (superior), and cricoid cartilage (inferior)—form the major structure of the larynx. The thyroid cartilage is the largest piece of cartilage that makes up the larynx. The thyroid cartilage consists of the laryngeal prominence, or “Adam’s apple,” which tends to be more prominent in males. The thick cricoid cartilage forms a ring, with a wide posterior region and a thinner anterior region. Three smaller, paired cartilages attach to the epiglottis, vocal cords and muscle that help move the vocal cords to produce speech.
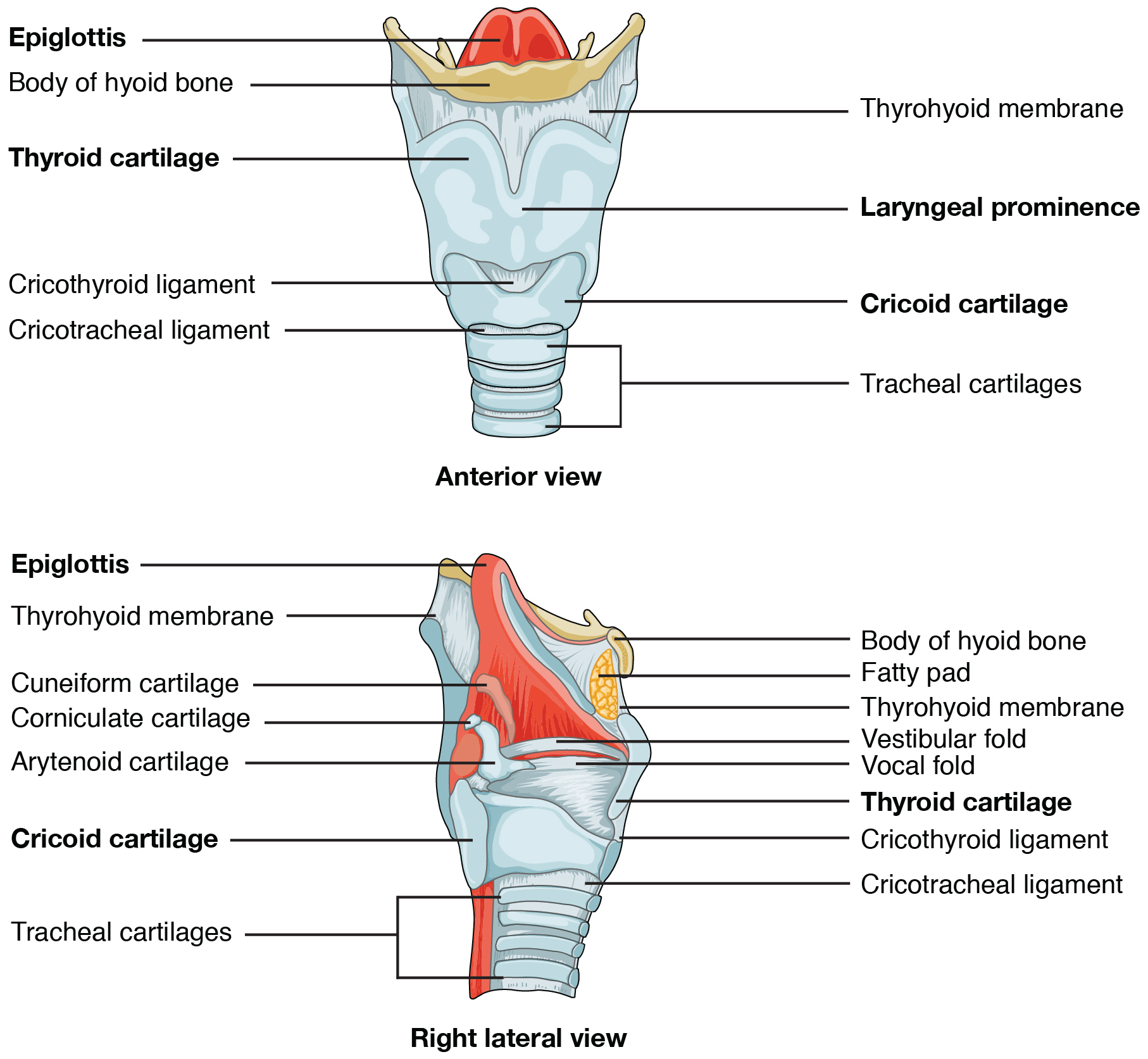
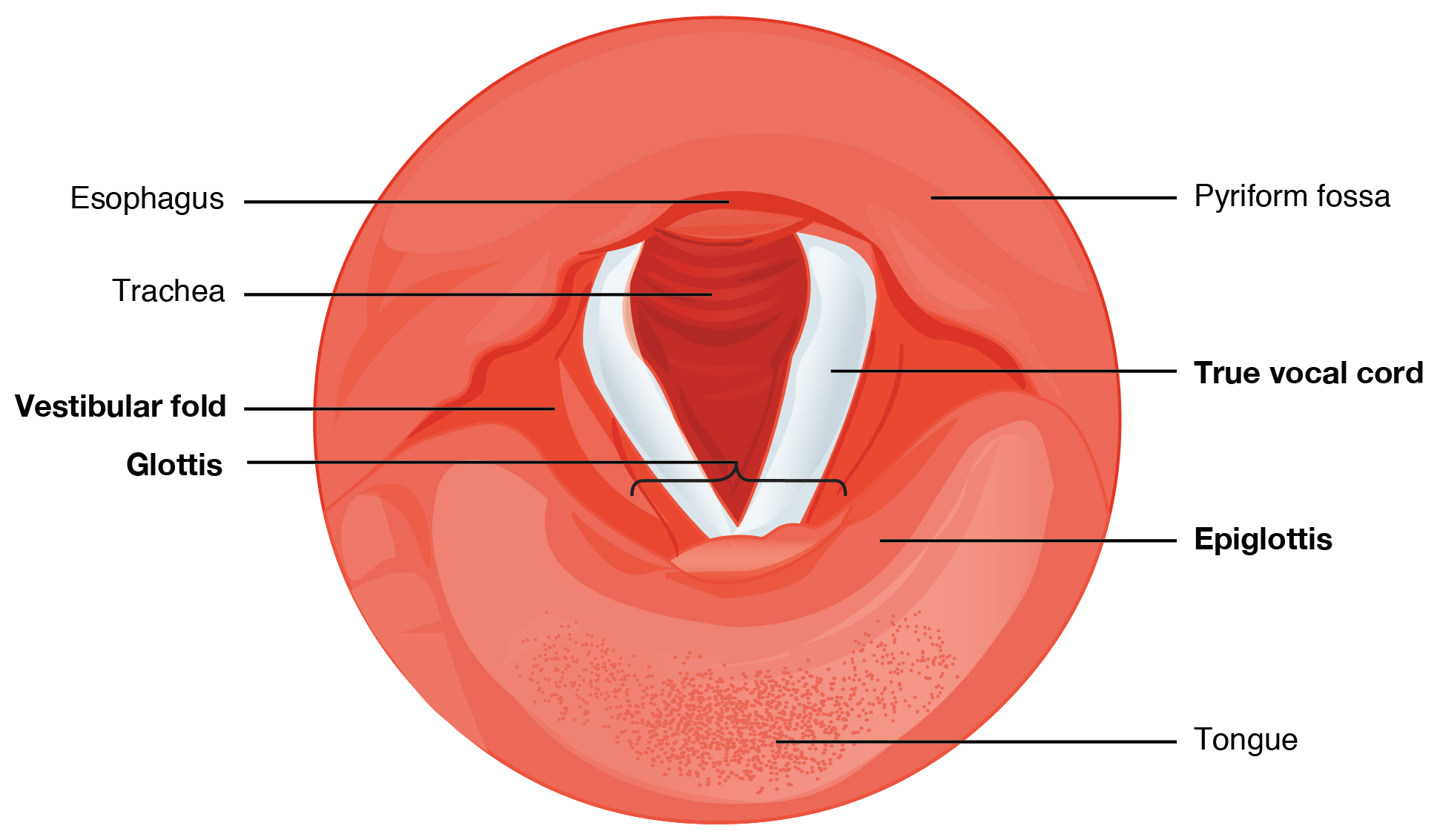
The epiglottis, attached to the thyroid cartilage, is a very flexible piece of elastic cartilage that covers the opening of the trachea during swallowing (Figure 12.1.4). When in the “closed” position, the unattached end of the epiglottis rests on the glottis. The glottis is composed of the vestibular folds, the true vocal cords, and the space between these folds (Figure 12.1.6). A vestibular fold is one of a pair of folded sections of mucous membrane. A true vocal cord is one of the white, membranous folds attached by muscle to the cartilages of the larynx on their outer edges. The inner edges of the true vocal cords are free, allowing oscillation to produce sound. The size of the membranous folds of the true vocal cords differs between individuals, producing voices with different pitch ranges. During puberty in males, higher levels of testosterone cause the vocal folds to thicken and the larynx to descend and thicken, typically resulting in a deepening of the voice.
The act of swallowing causes the pharynx and larynx to lift upward, allowing the pharynx to expand and the epiglottis of the larynx to swing downward, closing the opening to the trachea. These movements produce a larger area for food to pass through, while preventing food and beverages from entering the trachea.
Continuous with the laryngopharynx, the superior portion of the larynx is lined with stratified squamous epithelium, transitioning into pseudostratified ciliated columnar epithelium that contains goblet cells. Similar to the nasal cavity and nasopharynx, this specialized epithelium produces mucus to trap debris and pathogens as they enter the trachea. The cilia beat the mucus upward towards the laryngopharynx, where it can be swallowed down the esophagus.
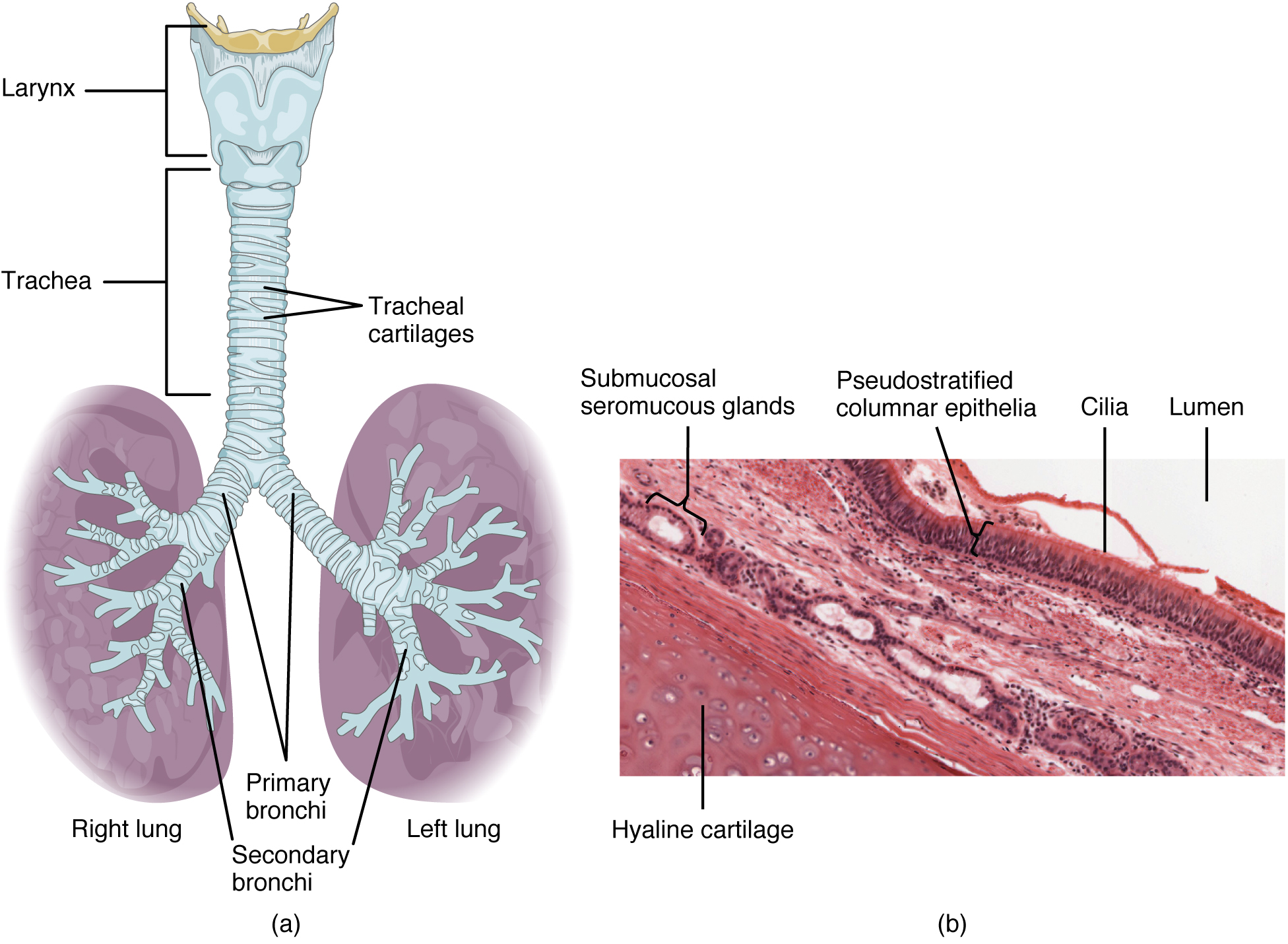
Trachea
The trachea (windpipe) extends from the larynx toward the lungs (Figure 12.1.7). The trachea is formed by 16 to 20 stacked, C-shaped pieces of hyaline cartilage that are connected by dense connective tissue. The trachealis muscle and elastic connective tissue together form the fibroelastic membrane, a flexible membrane that closes the posterior surface of the trachea, connecting the C-shaped cartilages. The fibroelastic membrane allows the trachea to stretch and expand slightly during inhalation and exhalation, whereas the rings of cartilage provide structural support and prevent the trachea from collapsing. In addition, the trachealis muscle can be contracted to force air through the trachea during exhalation. The trachea is lined with pseudostratified ciliated columnar epithelium, which is continuous with the larynx. The esophagus borders the trachea posteriorly.

Bronchi and Bronchial Tree
The trachea branches into the right and left primary bronchi (singular bronchus) at the carina, a ridge of cartilage at the base of the trachea. The mucous membrane of the carina is highly sensitive and is crucial in triggering coughing. If a foreign body, such as food, is present in this area, sensory nerve fibers fire impulses which in turn initiate the cough reflex.
The bronchi, like the trachea, are lined by pseudostratified ciliated columnar epithelium containing mucus-producing goblet cells (Figure 12.1.7). Rings of cartilage, similar to those of the trachea, support the structure of the bronchi and prevent their collapse. The primary bronchi enter the lungs at the hilum, a concave region where blood vessels, lymphatic vessels, and nerves also enter the lungs. The bronchi continue to branch into the bronchial tree. The bronchial tree (or respiratory tree) consists of a series of branching tubes that become narrower and shorter but more numerous as they descend into the lung (Figure 12.1.9).
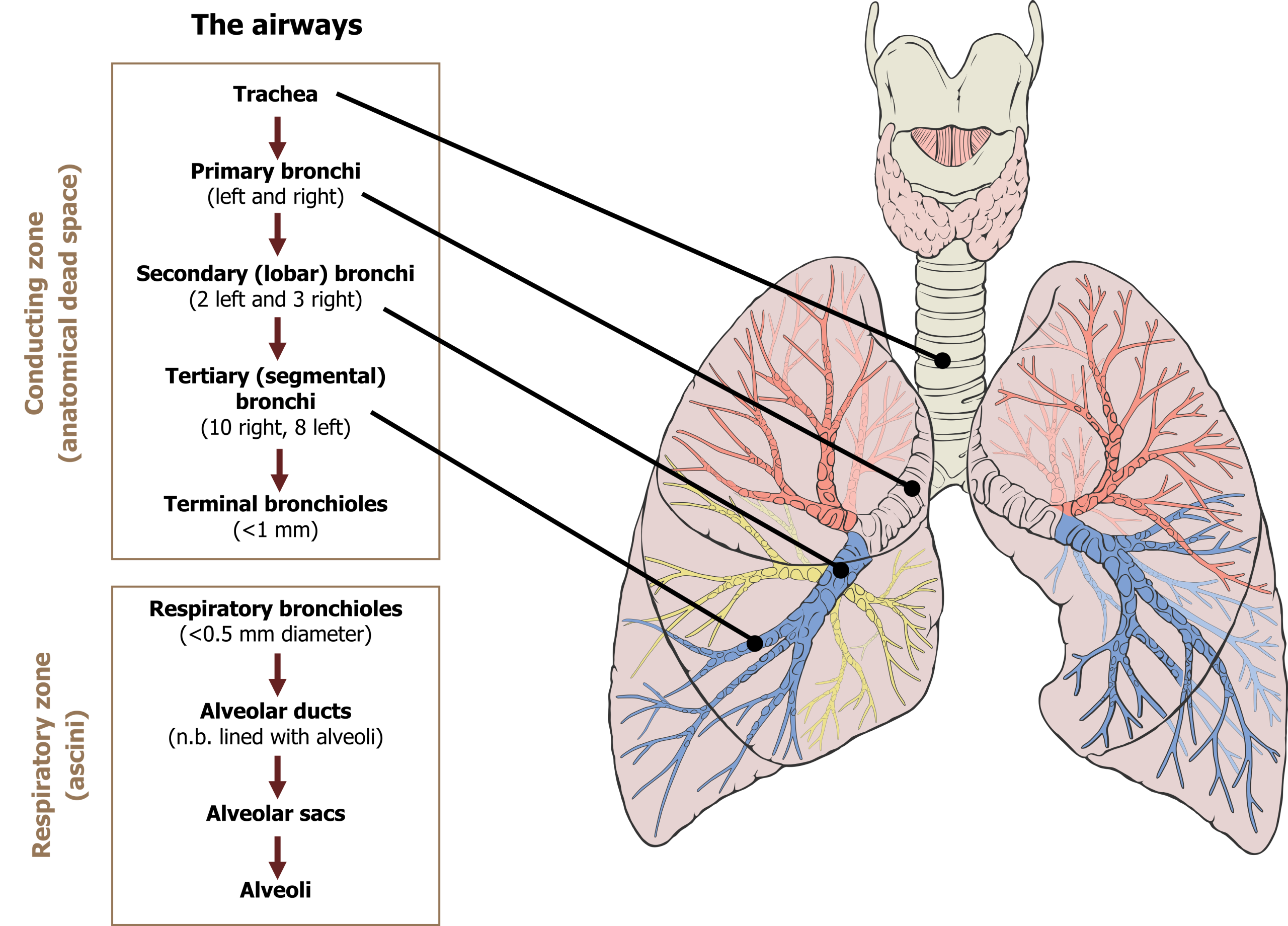
Bronchioles branch from the tertiary bronchi. Bronchioles, which are less than 1 mm in diameter, further branch until they become the tiny terminal bronchioles, which lead to the structures of gas exchange (Figure 12.1.9). There are more than 1,000 terminal bronchioles in each lung. The muscular walls of the bronchioles do not contain cartilage like those of the bronchi. Relaxation or contraction of the bronchiolar smooth muscle can change the diameters of the bronchioles to increase or decrease airflow.
Respiratory Zone Structures
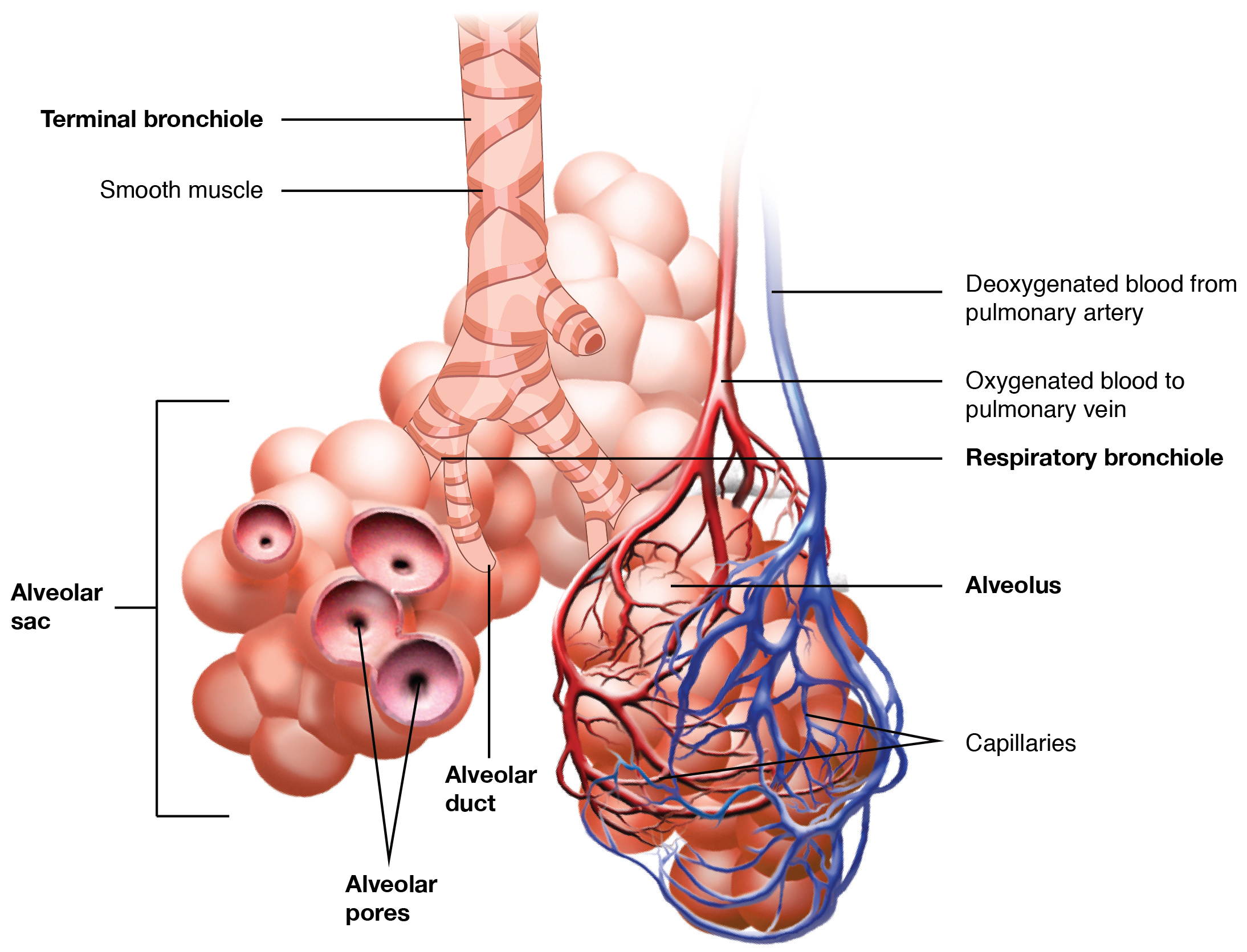
In contrast to the conducting zone, the respiratory zone includes structures that are directly involved in gas exchange. The respiratory zone begins where the terminal bronchioles join a respiratory bronchiole, the smallest type of bronchiole (Figure 12.1.10), which then leads to an alveolar duct, opening into a cluster of alveoli (alveolar sac).
Alveoli
An alveolar duct is a tube composed of smooth muscle and connective tissue, which opens into a cluster of alveoli. An alveolus is one of the many small, grape-like sacs that are attached to the alveolar ducts.
An alveolar sac is a cluster of many individual alveoli that are responsible for gas exchange. An alveolus is approximately 200 micrometers (μm) in diameter with elastic walls that allow the alveolus to stretch during air intake, which greatly increases the surface area available for gas exchange. Alveoli are connected to their neighbors by alveolar pores, which help maintain equal air pressure throughout the alveoli and lung (Figure 12.1.11).
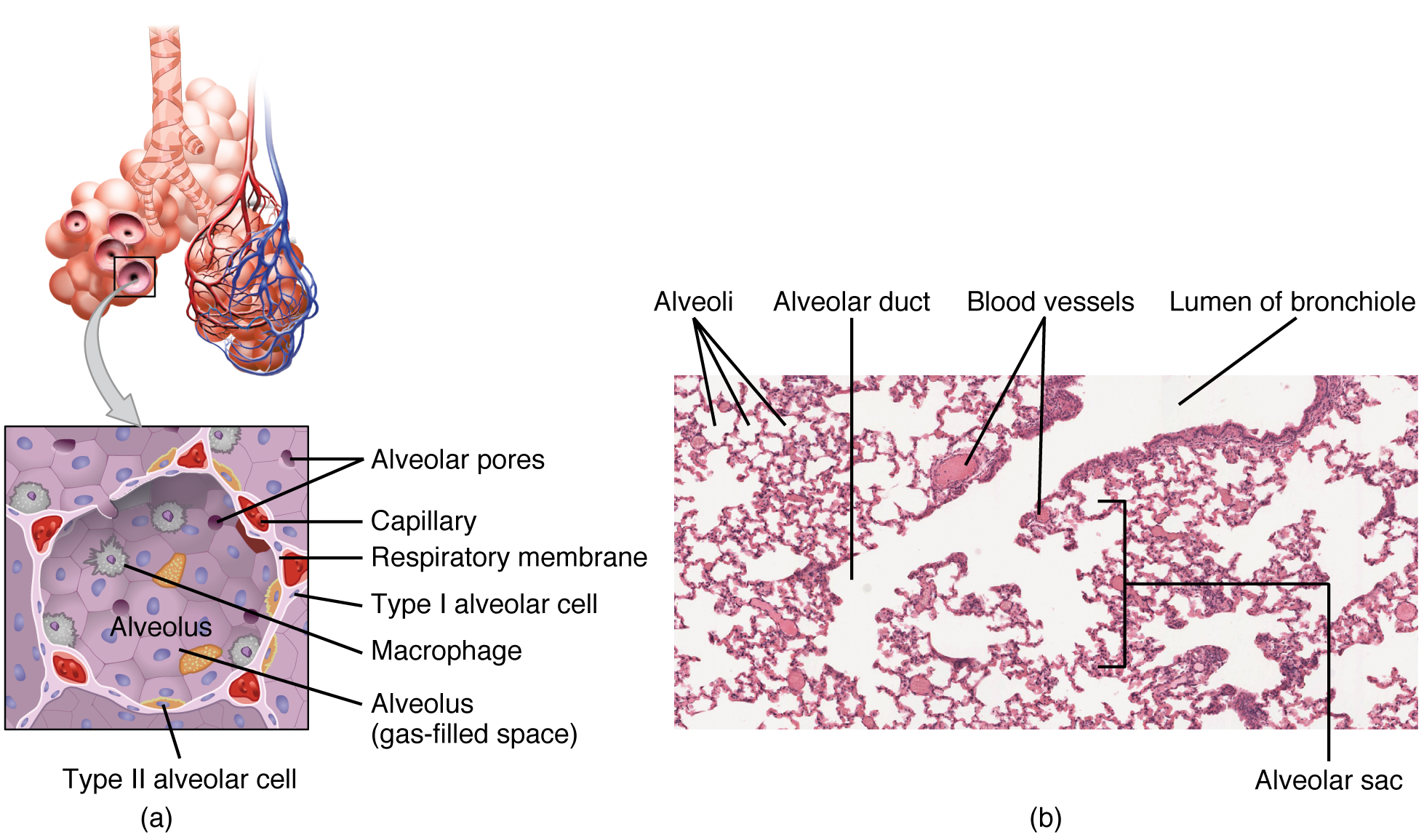
The alveolar wall consists of three major cell types: type I alveolar cells, type II alveolar cells, and alveolar macrophages. A type I alveolar cell is a squamous epithelial cell of the alveoli, which constitute up to 97% of the alveolar surface area. These cells are about 25 nanometers thick and are highly permeable to gases. A type II alveolar cell is interspersed among the type I cells and secretes pulmonary surfactant, a substance composed of phospholipids and proteins. Surfactant reduces the surface tension within the alveoli, which helps prevent the alveoli from collapsing. Roaming around the alveolar wall is the alveolar macrophage, a phagocytic cell of the immune system that removes debris and pathogens that have reached the alveoli.
The simple squamous epithelium formed by type I alveolar cells is attached to a thin, elastic basement membrane. Type I alveolar epithelium is extremely thin and borders the endothelial membrane of capillaries. Taken together, the type I epithelium and capillary endothelium form a respiratory membrane that is approximately 0.5 – 1.0 μm thick (1 μm = 10-6 m). The respiratory membrane allows gases to cross by simple diffusion, allowing oxygen to diffuse into the blood for transport and CO2 to be released into the air of the alveoli.
The major organs of the respiratory system, the lungs, house structures of both the conducting and respiratory zones and are discussed in the next section.
Disorders of the Respiratory System – Respiratory Distress Syndrome
Respiratory distress syndrome (RDS) is the most common cause of respiratory distress in premature infants. It results from insufficient production of pulmonary surfactant, thereby preventing the lungs from properly inflating at birth. Fetal lungs begin synthesizing surfactant after the 26th week of pregnancy, so babies born earlier than this are susceptible to developing RDS.
In babies with RDS, blood O2 levels are low and blood CO2 levels are high. In turn, high blood CO2 can lead to an acidosis in babies with RDS. While the primary cause of RDS is premature birth, other risk factors include gestational diabetes, cesarean delivery, second-born twins, and family history of RDS. The presence of RDS can lead to other serious disorders, such as septicemia (infection of the blood) or pulmonary hemorrhage. Therefore, it is important that RDS is immediately recognized and treated to prevent death and reduce the risk of developing other disorders.
Medical advances have resulted in an improved ability to treat RDS and support the infant until proper lung development can occur. At the time of delivery, treatment may include resuscitation and intubation if the infant is not able to breathe on their own. These infants would need to be placed on a ventilator to mechanically assist with the breathing process. If spontaneous breathing is occurring, application of nasal continuous positive airway pressure (CPAP) may be required. In addition, pulmonary surfactant is typically administered. Other therapies may include corticosteroids, supplemental oxygen, and assisted ventilation. Supportive therapies, such as temperature regulation, nutritional support, and antibiotics, may be administered to the premature infant as well.
Diseases of the Respiratory System – Asthma
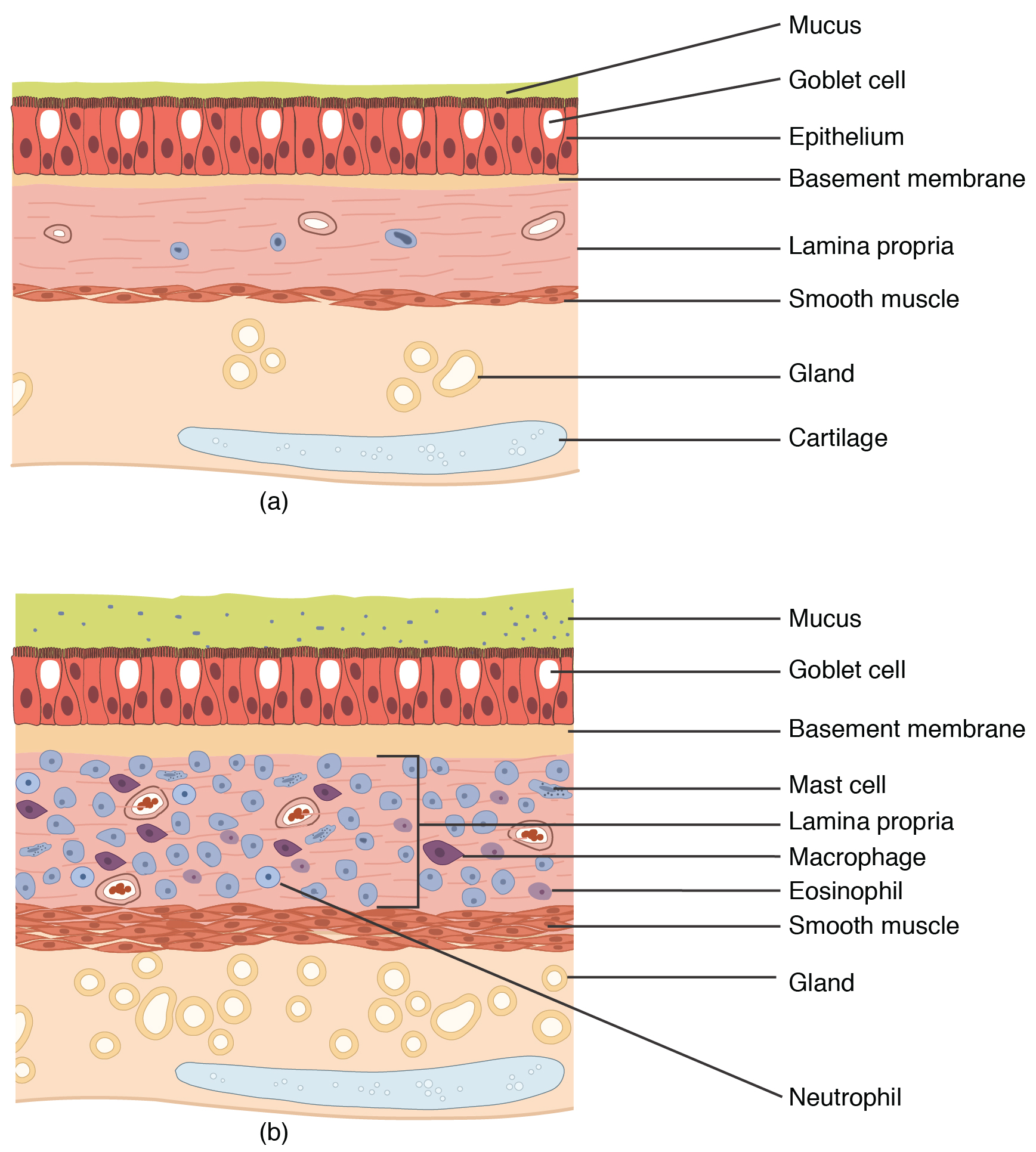
Asthma is a chronic disease characterized by inflammation and edema of the airway and bronchospasms (constriction of the bronchioles), which can prevent air from entering the lungs. In addition, excessive mucus secretion can occur, which further contributes to airway occlusion (Figure 12.1.12). The bronchiole hyperreactivity, increased mucus production, and airway inflammation characteristic of asthma ultimately result from a multifaceted immune response to allergens. In many cases, the underlying cause of the condition is unknown. However, recent research has demonstrated that certain viruses, such as human rhinovirus C (HRVC) and the bacteria Mycoplasma pneumoniae and Chlamydia pneumoniae that are contracted in infancy or early childhood, may contribute to the development of many cases of asthma.
The periodic bronchospasms can lead to an “asthma attack.” Asthma attack triggers include environmental factors such as dust, pollen, pet hair or dander, changes in the weather, mold, tobacco smoke, and respiratory infections. Certain non-environmental factors such as exercise and stress can also be triggers for an attack.
Symptoms of an asthma attack involve coughing, shortness of breath, wheezing, and tightness of the chest. Symptoms of a severe asthma attack that requires immediate medical attention would include difficulty breathing that results in blue (cyanotic) lips or face, confusion, drowsiness, a rapid pulse, sweating, and severe anxiety. The severity of the condition, frequency of attacks, and identified triggers influence the type of medication that an individual may require. Longer-term treatments are used for those with more severe asthma. Short-term, fast-acting drugs that are used to treat an asthma attack are typically administered via an inhaler. For young children or individuals who have difficulty using an inhaler, asthma medications can be administered via a nebulizer.
External Website
Section Review
The respiratory system is responsible for obtaining oxygen and eliminating carbon dioxide, maintaining acid-base balance, aiding in speech production and in sensing odors. From a functional perspective, the respiratory system can be divided into two major areas: the conducting zone and the respiratory zone.
The conducting zone consists of all of the structures that provide passageways for air to travel into and out of the lungs: the nasal cavity, pharynx, larynx, trachea, bronchi, and most bronchioles. The nasal passages warm and humidify incoming air, while removing debris and pathogens. The pharynx, an area common to the respiratory and digestive systems, leads to the larynx which contains the vocal folds.
The respiratory zone includes the structures of the lung that are directly involved in gas exchange: the terminal bronchioles and alveoli.
The mucosal lining of the conducting zone is composed mostly of pseudostratified ciliated columnar epithelium with goblet cells. The mucus traps pathogens and debris, whereas beating cilia move the mucus superiorly toward the throat, where it is swallowed. As the bronchioles become smaller and nearer the alveoli, the mucosal epithelium thins and transitions to simple squamous epithelium in the alveoli. The endothelium of the surrounding capillaries and the alveolar epithelium form the respiratory membrane, the site where gas exchange occurs by simple diffusion.
Review Questions
Critical Thinking Questions
Glossary
- alveolar macrophage
- immune system cell of the alveolus that removes debris and pathogens
- alveolus
- small, grape-like sac that performs gas exchange in the lungs
- bronchial tree
- collective name for the multiple branches of the bronchi and bronchioles of the respiratory system
- bronchiole
- branch of bronchi that are 1 mm or less in diameter and terminate at alveolar sacs
- bronchus
- tube connected to the trachea that branches into many subsidiaries and provides a passageway for air to enter and leave the lungs
- conducting zone
- region of the respiratory system that includes the organs and structures that provide passageways for air and are not directly involved in gas exchange
- epiglottis
- leaf-shaped piece of elastic cartilage that is a portion of the larynx that swings to close the trachea during swallowing
- glottis
- opening between the vocal folds through which air passes when producing speech
- larynx
- cartilaginous structure that contains the vocal folds
- nares
- the nostrils (singular naris)
- paranasal sinus
- one of the cavities within the skull that is connected to the conchae that serve to warm and humidify incoming air, produce mucus, and lighten the weight of the skull; consists of frontal, maxillary, sphenoidal, and ethmoidal sinuses
- pharynx
- region of the conducting zone that forms a tube of skeletal muscle lined with respiratory epithelium; located between the nasal conchae and the esophagus and trachea
- pulmonary surfactant
- substance composed of phospholipids and proteins that reduces the surface tension of the alveoli; made by type II alveolar cells
- respiratory bronchiole
- specific type of bronchiole that leads to alveolar sacs
- respiratory membrane
- alveolar type I epithelium and capillary endothelium together, which form an air-blood barrier that facilitates the simple diffusion of gases
- respiratory zone
- includes structures of the respiratory system that are directly involved in gas exchange
- trachea
- tube composed of cartilaginous rings and supporting tissue that connects the lung bronchi and the larynx; provides a route for air to enter and exit the lung
- true vocal cord
- one of the pair of folded, white membranes that have a free inner edge that oscillates as air passes through to produce sound
- type I alveolar cell
- squamous epithelial cells that are the major cell type in the alveolar wall; highly permeable to gases
- type II alveolar cell
- cuboidal epithelial cells that are the minor cell type in the alveolar wall; secrete pulmonary surfactant
Glossary Flashcards
References
Bizzintino, J., Lee, W. M., Laing, I. A., Vang, F., Pappas, T., Zhang, G., Martin, A. C., Khoo, S. K., Cox, D. W., Geelhoed, G. C., et al. (2010). Association between human rhinovirus C and severity of acute asthma in children. Eur Respir J 37(5):1037–1042.
Kumar, V., Cotran, R. S., & Robbins, S. L. (2003). Robbins basic pathology (7th ed.). Saunders.
Martin, R. J., Kraft, M., Chu, H. W., Berns, E. A., & Cassell, G. H. (2001). A link between chronic asthma and chronic infection. J Allergy Clin Immunol 107(4):595–601.
U.S. Department of Health and Human Services. (2022, March 24). Respiratory distress syndrome (RDS). National Heart Lung and Blood Institute.
This work, Human Physiology, is adapted from Anatomy & Physiology by OpenStax, licensed under CC BY, and Pulmonary Physiology for Pre-Clinical Students by Andrew Binks, licensed under CC BY-NC-SA. This edition, with revised content and artwork, is licensed under CC BY-SA except where otherwise noted.
Images from Anatomy & Physiology by OpenStax are licensed under CC BY except where otherwise noted.
Access the original for free at OpenStax.
Report an Error
Did you find an error, typo, broken link, or other problem in the text? Please follow this link to the error reporting form to submit an error report to the authors.
