Chapter 12. The Respiratory System
12.2 The Lungs
Learning Objectives
By the end of this section, you will be able to:
- state the overall function of the lungs;
- summarize the blood flow pattern associated with the lungs;
- explain the structural and functional relationships of the visceral and parietal pleura (pleural sacs), pleural fluid, thoracic cage, and lungs; and
- explain the importance of the surface tension in the pleural cavity.
A major organ of the respiratory system, each lung houses structures of both the conducting and respiratory zones. The main function of the lungs is to perform the exchange of oxygen and carbon dioxide with air from the atmosphere, and their anatomy makes them well-adapted for this task: typically a pair of human lungs has 300 to 500 million alveoli with a total surface area for gas exchange of 70 to 100 square meters!
Gross Anatomy of the Lungs
The lungs are pyramid-shaped, paired organs that are connected to the trachea by the right and left bronchi; on the inferior surface, the lungs are bordered by the diaphragm. The diaphragm is the flat, dome-shaped muscle located at the base of the lungs and thoracic cavity. The lungs are enclosed by the pleurae, which are attached to the mediastinum. The right lung is shorter and wider than the left lung, and the left lung occupies a smaller volume than the right. The cardiac notch is an indentation on the surface of the left lung, and it allows space for the heart (Figure 12.2.1). The apex of the lung is the superior region, whereas the base is the opposite region near the diaphragm. The costal surface of the lung borders the ribs. The mediastinal surface faces the midline.

Each lung is composed of smaller units called lobes. Fissures separate these lobes from each other. The right lung consists of three lobes: the superior, middle, and inferior lobes. The left lung consists of two lobes: the superior and inferior lobes. A bronchopulmonary segment is a division of a lobe, and each lobe houses multiple bronchopulmonary segments. Each segment receives air from its own tertiary bronchus and is supplied with blood by its own artery. Some diseases of the lungs typically affect one or more bronchopulmonary segments, and in some cases, the diseased segments can be surgically removed with little influence on neighboring segments. A pulmonary lobule is a subdivision formed as the bronchi branch into bronchioles. Each lobule receives its own large bronchiole that has multiple branches. An interlobular septum is a wall, composed of connective tissue, which separates lobules from one another.
Blood Supply and Nervous Innervation of the Lungs
The blood supply to the lungs plays an important role in gas exchange. In addition, innervation by the both the parasympathetic and sympathetic nervous systems provides an important level of control through dilation and constriction of the airways.
Blood Supply (Pulmonary Circulation)
The circuit of blood vessels supplying the lungs is the pulmonary circulation, or pulmonary circuit. Blood vessels of the pulmonary circuit deliver deoxygenated blood to the lungs, where it is oxygenated, and then transport oxygenated blood to the left side of the heart, which pumps the freshly oxygenated blood to the body and cardiac muscle via the systemic and coronary circuits.
General Anatomy of the Pulmonary Circulation
The left and right pulmonary arteries arise from the pulmonary trunk and carry deoxygenated blood to the lungs. The pulmonary arteries branch into lobar arteries that follow the main bronchi as they enter the lungs. The arteries branch multiple times, first forming arterioles and then pulmonary capillary networks that surround the alveoli. The pulmonary capillaries are the sites of gas exchange. Specifically, as mentioned previously, the endothelium of the pulmonary capillaries and the type I alveolar cell epithelium form the respiratory membrane across which gas exchange occurs. Once the blood is oxygenated, it drains from the alveoli by way of multiple pulmonary venules and eventually pulmonary veins, which carry oxygenated blood to the left atrium of the heart.
Nervous Innervation
Dilation and constriction of the airway are achieved through nervous control by the parasympathetic and sympathetic nervous systems. The parasympathetic system causes contraction of the bronchiolar smooth muscle, resulting in bronchoconstriction, a decrease in the diameter of bronchioles; the sympathetic nervous system stimulates relaxation of the bronchiolar smooth muscle, resulting in bronchodilation, an increase in the diameter of bronchioles. Reflexes such as coughing, and the ability of the lungs to regulate oxygen and carbon dioxide levels, also result from autonomic nervous system control. Sensory nerve fibers arise from the vagus nerve, and from the second to fifth thoracic ganglia. The pulmonary plexus is a region on the lung root formed by the entrance of the nerves at the hilum. The nerves then follow the bronchi in the lungs and branch to innervate muscle fibers, glands, and blood vessels.
Pleurae of the Lungs
Each lung is enclosed within a cavity that is surrounded by the pleura. The pleura (plural = pleurae) is a serous membrane that surrounds the lung. The right and left pleurae, which enclose the right and left lungs, respectively, are separated by the mediastinum. The pleurae consist of two layers. The visceral pleura is the layer that is superficial to the lungs, and extends into and lines the lung fissures (Figure 12.2.2). In contrast, the parietal pleura is the outer layer that connects to the thoracic wall, the mediastinum, and the diaphragm. The visceral and parietal pleurae connect to each other at the hilum. The pleural cavity is the space between the visceral and parietal layers.
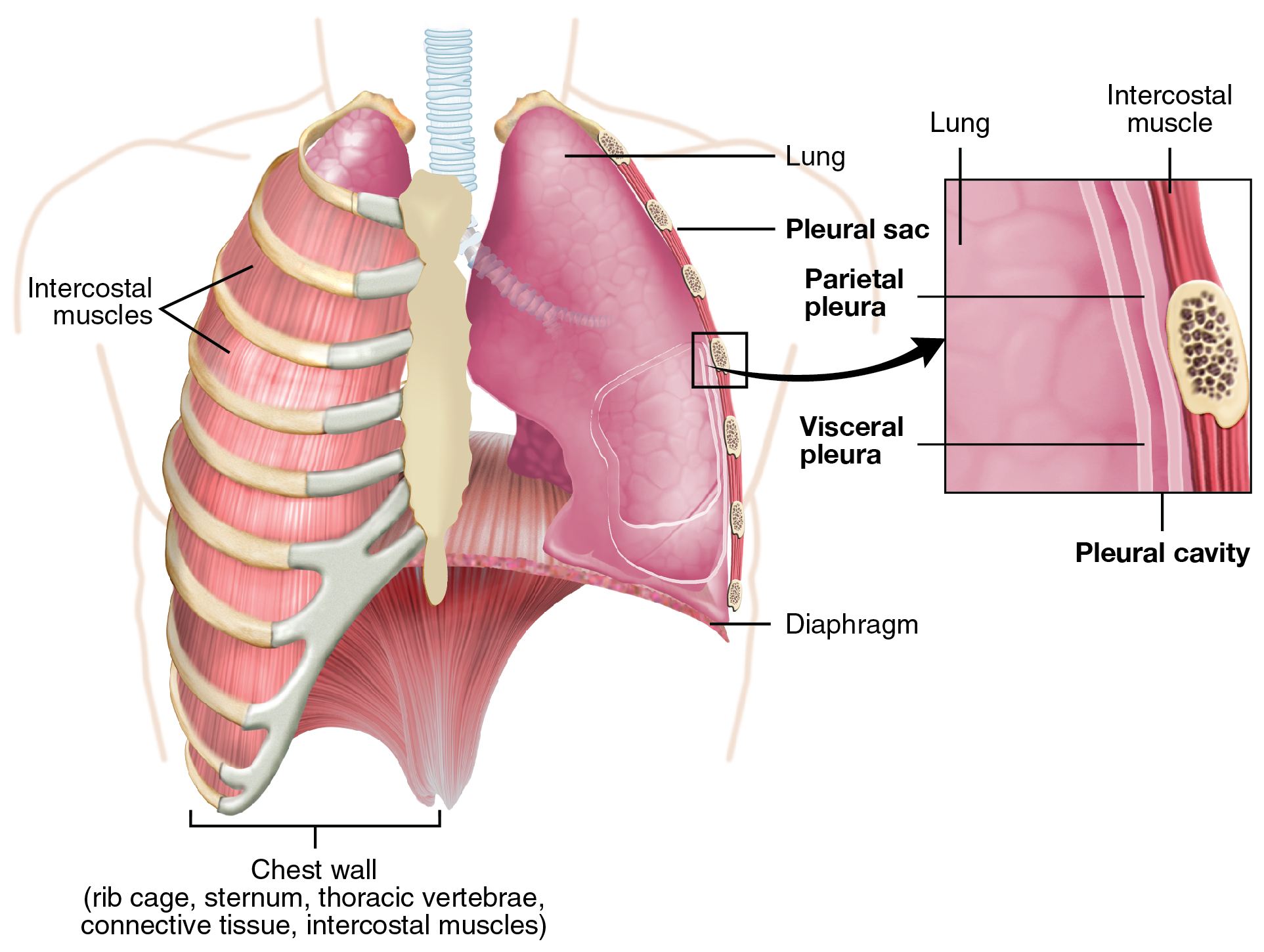
The pleurae perform two major functions: They produce pleural fluid and create cavities that separate the major organs. Pleural fluid is secreted by mesothelial cells from both pleural layers and acts to lubricate their surfaces, reducing friction between the two layers to prevent trauma during breathing. The pleurae also create a division between major organs that prevents interference due to the movement of the organs, while preventing the spread of infection.
Another vital function of the pleural fluid is that it creates surface tension in the pleural cavity that prevents the separation of the visceral and parietal pleurae. The surface tension of the pleural fluid is essential in that it causes the lungs to follow the movements of the thoracic wall during ventilation.
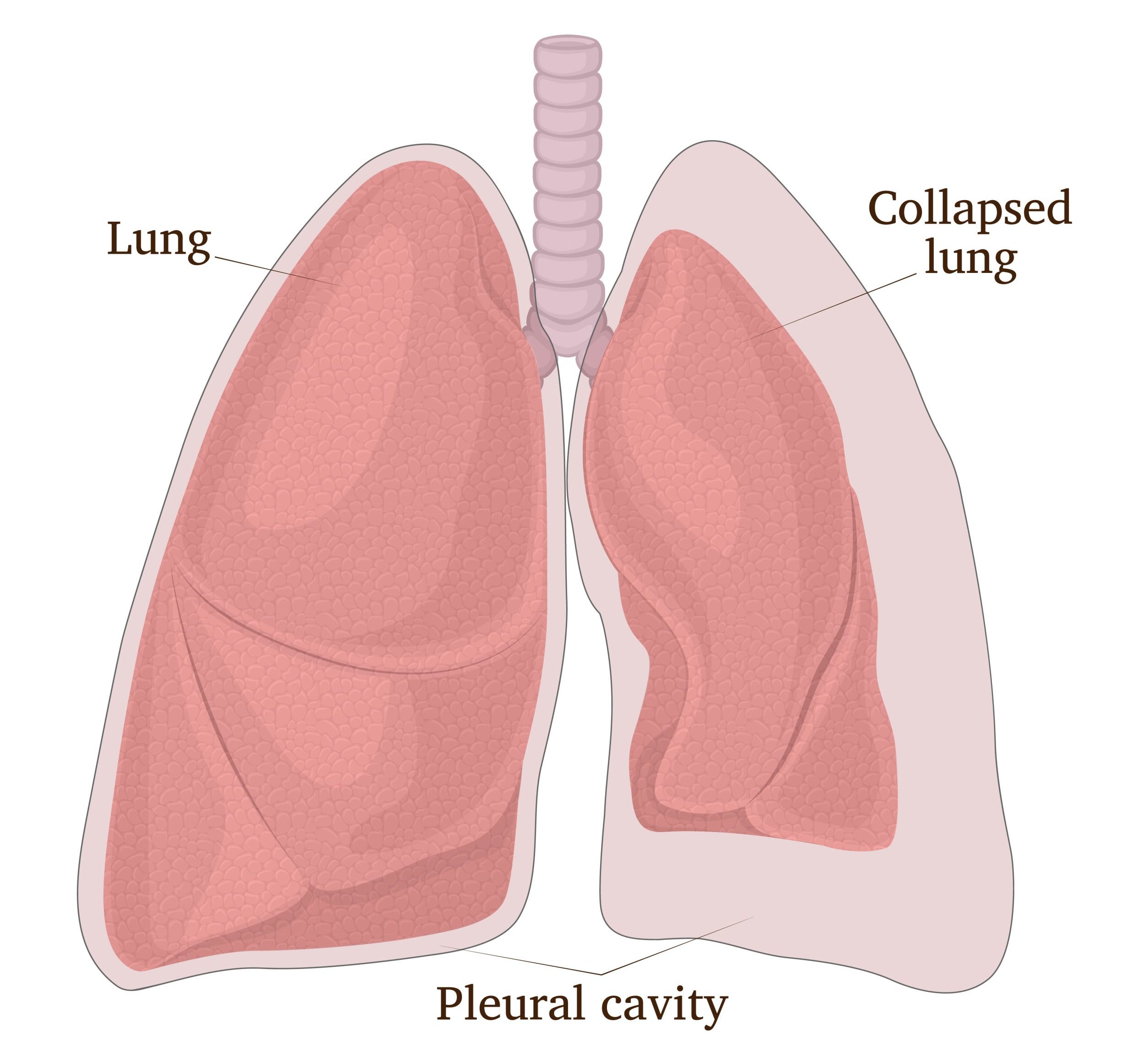
A pneumothorax, the presence of air in a pleural cavity, is a serious condition that can arise in several ways, including a wound to the chest or rupture of the pleurae (Figure 12.2.3.) A pneumothorax can lead to lung collapse (atelectasis) due to the loss of the surface tension and an equalization of pressure between the lung and pleural cavity or pleural cavity and atmosphere. The air pressures important in ventilation will be discussed in the next chapter section.
External Website
View the video below for an introduction to COPD (chronic obstructive pulmonary disease) and then read the more detailed explanation below. Click here to view “The Basics of Chronic Obstructive Pulmonary Disease (COPD)” by NHLBI (June 26, 2018) in a separate tab.
Diseases of the Respiratory System – COPD
Chronic bronchitis and emphysema comprise a group of diseases called chronic obstructive pulmonary disease, or COPD. In certain cases, asthma is included in COPD.
In emphysema, breakdown of the protein elastin occurs, which leads to the destruction of the walls between the alveoli and a loss of lung elasticity. Elastin is essential in allowing the lungs to recoil so as elastin is lost, the lungs lose their ability to recoil during ventilation.) As a result, patients need to recruit accessory muscles to breathe properly and can become exhausted. In addition, the loss of alveolar walls and loss of recoil prevents (obstructs) sufficient airflow into and out of the lungs.
In chronic bronchitis, thick mucus builds up in the airways as a result of repeated irritation of and inflammation of the linings of the airways. The mucus buildup decreases diameter of the airways, which increases airway resistance, obstructs airflow, and makes breathing more difficult.
According to the CDC, COPD is the sixth leading cause of death in the United States. The main factors that cause COPD are cigarette smoking and environmental pollution, but a rare genetic condition, alpha-1 antitrypsin (AAT) deficiency, is also a cause. If you are interested in reading more about AAT, click here.
Cigarette Smoking and Respiratory Diseases
The leading cause of preventable disease and death in the United States is cigarette smoking. In 2020, an estimated 28.3 million, or 12.5%, of U.S. adults reported regular cigarette smoking.
Cigarette smoking causes many diseases and harms almost every organ system in the body, including the respiratory system. Cancers of the respiratory system (mouth and throat, trachea, bronchi, and lung) and COPD are the main respiratory diseases caused by smoking. At least 69 of the over 7,000 chemicals found in cigarette smoke can cause cancer, and other chemicals in this large group have been shown to lessen the body’s ability to fight cancer. In addition, cigarette smoke also causes the airway irritation, inflammation, and alveolar damage characteristic of COPD.
The burning of a tobacco cigarette creates multiple chemical compounds that are released through mainstream smoke, which is inhaled by the smoker, and through sidestream smoke, which is the smoke given off by the burning cigarette. Second-hand smoke, which is a combination of sidestream smoke and the mainstream smoke that is exhaled by the smoker, has been demonstrated by numerous scientific studies to cause disease.
Tobacco and second-hand smoke are considered to be carcinogenic. Exposure to second-hand smoke can cause lung cancer in individuals who are not tobacco users themselves. It is estimated that the risk of developing lung cancer is increased by up to 30 percent in nonsmokers who live with an individual who smokes in the house, as compared to nonsmokers who are not regularly exposed to second-hand smoke. Children are especially affected by second-hand smoke. Children who live with an individual who smokes inside the home have a larger number of lower respiratory infections, a greater number of ear infections, as well as worsening symptoms of asthma. In addition, lung growth and development in children and teens can slow down as a result of smoking and exposure to secondhand smoke. This increases their risk of developing COPD as adults.
Clinical Connections – Respiratory Health Disparities
Respiratory diseases disproportionately affect marginalized populations and these disparities, as with other health disparities, originate from broader inequities and are closely linked to social, economic, and/or environmental disadvantages as well as racism. For example, a recent (2021) study comparing American Indian/Alaska Native (AI/AN) populations and non-Hispanic White populations revealed significant disparities in the incidence of chronic respiratory disease (Figure 12.2.4). In eight of the nine years analyzed by the study, the AI/AN population had a significantly higher prevalence of chronic respiratory disease than non-Hispanic White populations. The study further showed this inequality was strongly linked to disadvantages that are more prevalent in AI/AN populations than in White populations, namely poverty and having less than a high school education.
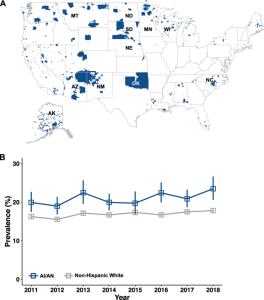
While this study specifically studied respiratory disease prevalence in AI/AN populations, much research has been done to examine health inequities in other non-white communities. For example, studies showed that 24.9 million people (7.7% of the U.S. population) suffered from asthma in the U.S. in 2021 and within this total, significant racial disparities in asthma prevalence were revealed. Non-Hispanic Black populations had the highest prevalence of asthma when compared to all other reporting races or ethnicities.
The causes of respiratory health disparities are myriad and are still being understood, but factors rooted in low socioeconomic status and racism contribute. Such factors include poor housing quality, adverse environmental exposures, reduced access to health care, and higher smoking rates in non-Hispanic Black populations. Although a decrease in the number of smokers in non-Hispanic Black populations occurred between 2011 and 2020 due in part to tobacco intervention programs, disparities still exist. In part, these can be linked to the increased selling of tobacco in neighborhoods with greater percentages of non-Hispanic Black and Hispanic residents. A systematic review of 20 years’ worth of studies conducted worldwide, published in 2024, revealed that neighborhoods with higher populations of Black and Hispanic residents saw significantly higher tobacco retailer availability. In addition, the directed marketing of tobacco products (via billboards, television ads, and so forth) to Black populations in the U.S. since the 1950s has been well documented.
Watch the video below to learn more about this targeted marketing from “Medical Mythbuster” and physician Joel Bervell. Click here to view “Big Tobacco has long targeted Black communities with menthol cigarettes. That has to stop.” by Joel Bervell (May 16, 2024) in a separate tab.
For more information on the history of targeted marketing of tobacco to Black communities, visit the links provided in the references below.
Section Review
The lungs are the major organs of the respiratory system and are responsible for performing gas exchange. The lungs are paired and separated into lobes; The left lung consists of two lobes, whereas the right lung consists of three lobes. The function of the pulmonary circulation is to facilitate gas exchange. The pulmonary arteries provide deoxygenated blood to the capillaries that form respiratory membranes with the alveoli, and the pulmonary veins return freshly oxygenated blood to the heart for further transport throughout the body. The lungs are innervated by the parasympathetic and sympathetic nervous systems, which coordinate the bronchodilation and bronchoconstriction of the airways. The lungs are enclosed by the pleura, a membrane that is composed of visceral and parietal pleural layers. The space between these two layers is called the pleural cavity. The mesothelial cells of the pleural membrane secrete pleural fluid into the pleural cavity, which serves as both a lubricant (to reduce friction during breathing) and as a source of surface tension to adhere the lungs to the thoracic wall and enable them to follow the movements of the thoracic wall during ventilation.
Review Questions
Critical Thinking Questions
Glossary
- bronchoconstriction
- decrease in the size of the bronchiole due to contraction of the muscular wall
- bronchodilation
- increase in the size of the bronchiole due to contraction of the muscular wall
- cardiac notch
- indentation on the surface of the left lung that allows space for the heart
- chronic obstructive pulmonary disease
- a group of respiratory diseases comprised of chronic bronchitis, emphysema, and, in certain cases, asthma
lung
organ of the respiratory system that performs gas exchange
- parietal pleura
- outermost layer of the pleura that lines the thoracic wall, mediastinum, and diaphragm
- pleural cavity
- space between the visceral and parietal pleurae
- pleural fluid
- substance that acts as a lubricant for and that creates surface tension between the visceral and parietal layers of the pleura during the movement of breathing
- pneumothorax
- presence of air in a pleural cavity
- pulmonary circulation
- circuit of blood vessels that supplies the lungs
- pulmonary arteries
- arteries that arises from the pulmonary trunk and carry deoxygenated blood to the lungs
- pulmonary capillaries
- smallest blood vessels in the pulmonary circulation; vessel wall consist only of endothelium; site of gas exchange
- pulmonary veins
- veins that carry oxygenated blood from the lungs to the left atrium
- visceral pleura
- innermost layer of the pleura that is superficial to the lungs and extends into the lung fissures
Glossary Flashcards
References
Arrazola, R. A., Griffin, T., Lunsford, N. B., Kittner, D., Bammeke, P., Courtney-Long, E. A., et al. (2023). US Cigarette Smoking Disparities by Race and Ethnicity — Keep Going and Going!. Preventing Chronic Disease 20:220375.
Centers for Disease Control and Prevention. (n.d.). About COPD. Centers for Disease Control and Prevention.
Cornelius, M. E., Loretan, C. G., Wang, T. W., Jamal, A., & Homa, D. M. (2020). Tobacco Product Use Among Adults — United States. Morb Mortal Wkly Rep 2022(71):397–405.
Grant, T., Croce, E., & Matsui, E. C. (2022). Asthma and the Social Determinants of Health. Annals of Allergy, Asthma & Immunology 128(1):5–11.
Laffey, K. G., Nelson, A. D., Laffey, M. J., Nguyen, Q., Sheets, L. R., & Schrum, A. G. (2021). Chronic respiratory disease disparity between American Indian/Alaska Native and White Populations, 2011–2018. BMC Public Health 21(1).
Pate, C. A., & Zahran, H. S. (2024). The Status of Asthma in the United States. Preventing Chronic Disease 21:240005.
Additional video resources regarding targeted marketing of tobacco in Black neighborhoods:
Centers for Disease Control and Prevention (CDC). (2014, September 12). Unequal opportunity killer [Video].
Mondy, Lincoln. (2017, August 6). Black Lives/Black Lungs [Video].
This work, Human Physiology, is adapted from Anatomy & Physiology by OpenStax, licensed under CC BY. This edition, with revised content and artwork, is licensed under CC BY-SA except where otherwise noted.
Images from Anatomy & Physiology by OpenStax are licensed under CC BY except where otherwise noted.
Access the original for free at OpenStax.
Report an Error
Did you find an error, typo, broken link, or other problem in the text? Please follow this link to the error reporting form to submit an error report to the authors.
