Chapter 12. The Respiratory System
12.3 Pulmonary Ventilation
Learning Objectives
By the end of this section, you will be able to:
- define ventilation;
- define inspiration and expiration;
- list the muscles used during quiet inspiration and during forced inspiration and forced expiration;
- state the main determinant of ventilation;
- define atmospheric pressure, intra-alveolar pressure, intrapleural pressure, and transpulmonary pressure;
- discuss how gas pressures and volumes are related;
- explain how changes in lung volume affect intra-alveolar pressure;
- explain how changes in intra-alveolar pressure cause inspiration and expiration;
- explain how the actions of the respiratory muscles during ventilation lead to changes in lung volume and to changes in intra-alveolar pressure;
- define airway resistance and describe the effects of airway diameter on airway resistance;
- identify the sites of greatest resistance and of variable resistance in a healthy person;
- define lung compliance;
- define the four respiratory volumes: inspiratory reserve volume (IRV), tidal volume (TV), expiratory reserve volume (ERV), and residual volume (RV); and
- define the four respiratory capacities: inspiratory capacity (IC), functional residual capacity (FRC), vital capacity (VC), and total lung capacity (TLC).
Pulmonary ventilation is the act of breathing, which is the movement of air into and out of the lungs. Pulmonary ventilation comprises two major steps: inspiration and expiration. Inspiration (inhalation) is the process that causes air to enter the lungs, and expiration (exhalation) is the process that causes air to leave the lungs. A respiratory cycle is one sequence of inspiration and expiration.
The main determinant of air flow into and out of the lungs is a difference in air pressure between the atmosphere (atmospheric pressure, Patm) and inside the alveoli (intra-alveolar pressure, Palv). The pressure within the pleural cavity, intrapleural pressure (Pip), is another pressure important to ventilation. The difference in pressures drives pulmonary ventilation because air flows down a pressure gradient, from an area of higher pressure to an area of lower pressure. Air flows into the lungs when intra-alveolar pressure drops below atmospheric pressure. Air flows out of the lungs during expiration when intra-alveolar pressure becomes greater than the atmospheric pressure. These respiratory pressures (Patm, Palv, and Pip) will be discussed in more detail later in this section.
Rhythmic contraction and relaxation of the respiratory muscles enable inspiration and expiration. In order to fully understand how these activities of the respiratory muscles lead to ventilation, it is essential to understand the relationship between the volume of an pressure of a gas at a constant temperature.
Pressure-Volume Relationships
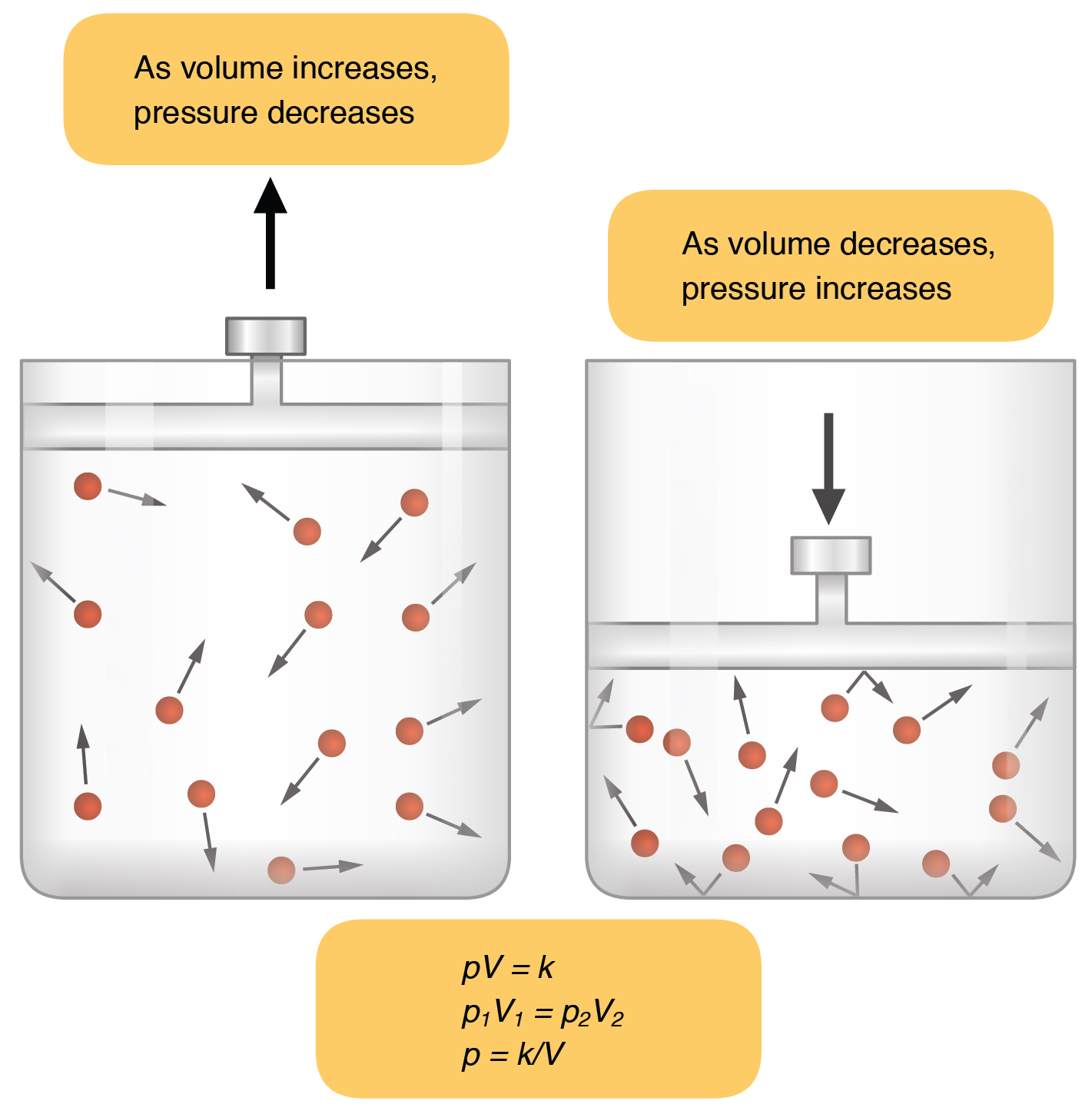
When referring to a gas, pressure is a force created by the movement of gas molecules that are confined. Increasing the number of gas molecules in a confined space will increase the pressure. At a constant temperature, changing the volume occupied by the gas changes the pressure, as does changing the number of gas molecules. Consider Figure 12.3.1, which shows two containers of different volume, each containing 13 molecules of a gas. The force exerted by the movement of the gas molecules against the walls of the larger container on the left is lower than the force exerted by the gas molecules in the container on the right. Therefore, the pressure is lower in the larger container and higher in smaller container.
Boyle’s law describes the relationship between the volume and pressure of a gas in a confined space. Specifically, the Law states that for a given mass of a gas in a confined space at a constant temperature, the product of the pressure and volume is also constant (“k” in the equation in Figure 12.3.1). Boyle’s Law is expressed by the following formula:
P1V1 = P2V2
In this formula, P1 represents the initial pressure and V1 represents the initial volume, whereas the final pressure and volume are represented by P2 and V2, respectively. In short, pressure and volume are inversely related.
Respiratory Pressures
Pulmonary ventilation is dependent on three pressures: atmospheric, intra-alveolar, and intrapleural. Atmospheric pressure is the amount of force that is exerted by gases in the air surrounding any given surface, such as the body. Atmospheric pressure can be expressed in terms of the unit atmosphere, abbreviated atm, or in millimeters of mercury (mm Hg). One atm is equal to 760 mm Hg, which is the atmospheric pressure at sea level. Typically, for ventilation, other pressure values are discussed in relation to atmospheric pressure. Therefore, negative pressure is pressure lower than the atmospheric pressure, whereas positive pressure is pressure that it is greater than the atmospheric pressure. A pressure that is equal to the atmospheric pressure is expressed as zero.
Intra-alveolar pressure is the pressure of the air within the alveoli, which changes during the different phases of breathing (Figure 12.3.2). Because the alveoli are connected to the atmosphere via the airways, intra-alveolar pressure always equalizes with atmospheric pressure.
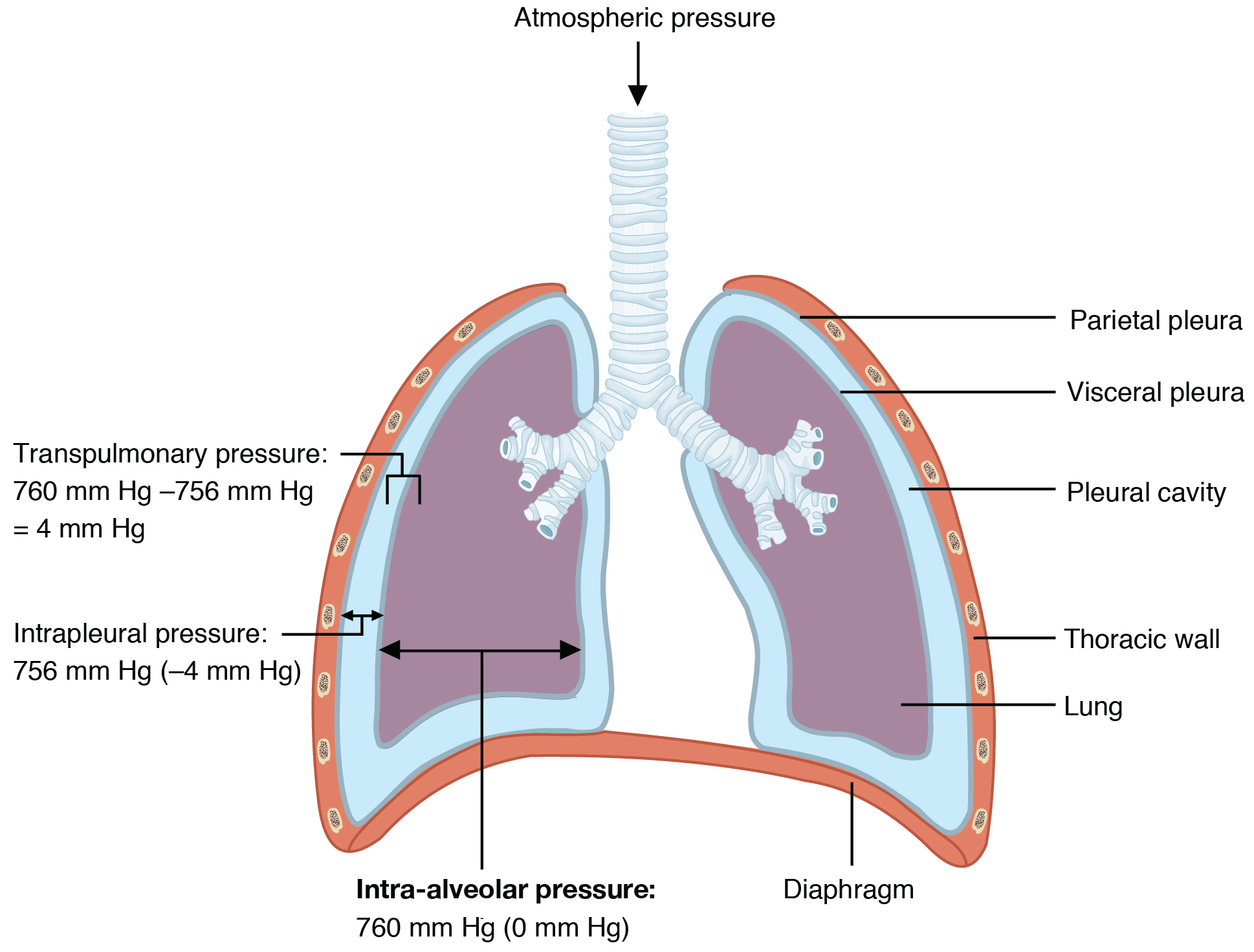
Intrapleural pressure (Pip) is the pressure within the fluid-filled pleural cavity. Similar to intra-alveolar pressure, intrapleural pressure also changes during the different phases of breathing. Although it fluctuates during inspiration and expiration, intrapleural pressure is always less than atmospheric pressure and intra-alveolar pressure. Pip remains approximately –4 mm Hg throughout the breathing cycle. Pip results from the surface tension between the visceral and parietal pleura and the parietal pleura’s adhesion to the body wall and diaphragm. Competing forces within the thorax cause the formation of the negative intrapleural pressure. One of these forces relates to the elasticity of the lungs themselves—elastic tissue pulls the lungs inward, away from the thoracic wall. Alveolar surface tension also creates an inward pull of the lung tissue. This inward tension from the lungs is countered by opposing forces from the pleural fluid and thoracic wall: surface tension within the pleural cavity pulls the lungs outward and the natural elasticity of the chest wall opposes the inward pull of the lungs. Ultimately, the outward pull is slightly greater than the inward pull, creating the –4 mm Hg intrapleural pressure relative to the intra-alveolar pressure.
Transpulmonary pressure is the difference between the intrapleural and intra-alveolar pressures. Transpulmonary pressure is always positive in a healthy respiratory system; this is essential in allowing the lungs to stay open.
In summary, two main forces keeping the lungs open are pleural fluid surface tension and positive transpulmonary pressure.
Respiratory Muscles and Pulmonary Ventilation
Recall that the main determinant of ventilation is a difference in air pressure between the atmosphere (atmospheric pressure, Patm) and inside the alveoli (intra-alveolar pressure, Palv). The regular contraction and relaxation of the respiratory muscles cause this air pressure difference; specifically, Palv changes as the respiratory muscles contract and relax.
Inspiration: Normal, Quiet Breathing
In general, two muscle groups are used during normal, quiet inspiration: the diaphragm and the external intercostal muscles. Inspiration is active: it involves muscle contraction. When the diaphragm contracts, it moves inferiorly toward the abdominal cavity, creating a larger thoracic cavity. At the same time, contraction of the external intercostal muscles moves the ribs upward and outward, causing the rib cage to expand, which increases the volume of the thoracic cavity. Due to the surface tension of the pleural fluid, the expansion of the thoracic cavity forces the lungs to stretch and expand as well. This increase in volume leads to a decrease in intra-alveolar pressure, creating a pressure lower than atmospheric pressure. As a result, a pressure gradient is created that drives air into the lungs.
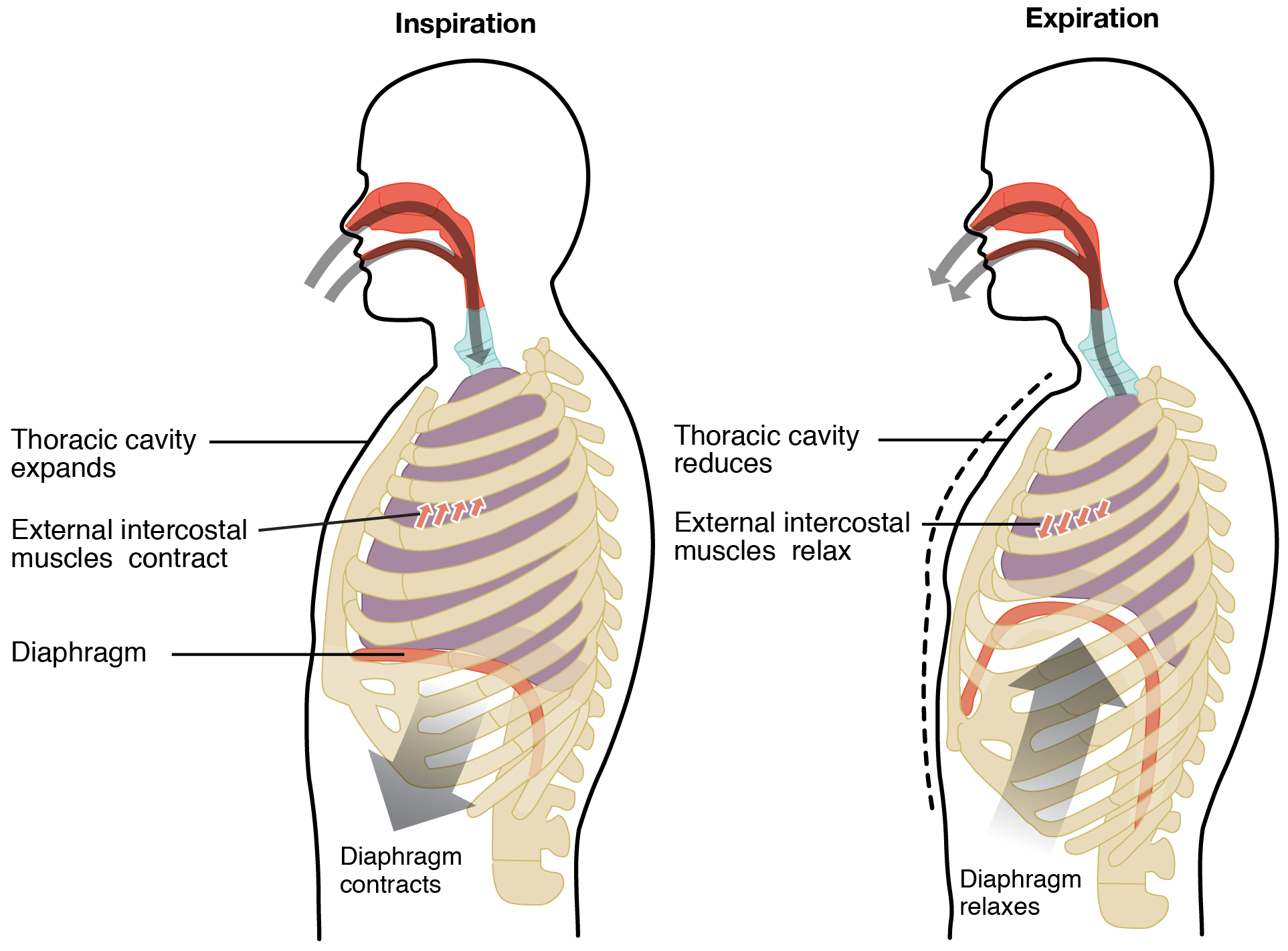
Expiration: Normal, Quiet Breathing
The process of normal, quiet expiration is passive, meaning that energy is not required to push air out of the lungs. Instead, the elasticity of the lung tissue causes the lung to recoil, as the diaphragm and intercostal muscles relax following inspiration. In turn, the thoracic cavity and lungs decrease in volume, causing an increase in intra-alveolar pressure. The intra-alveolar pressure rises above atmospheric pressure, creating a pressure gradient that causes air to leave the lungs.
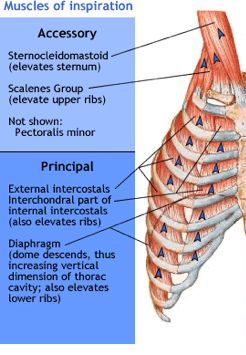
Inspiration and Expiration During Forced Breathing
During forced breathing, inspiration and expiration both occur due to muscle contractions. During periods of high ventilatory need (or drive), additional muscles can contribute to expansion of the rib cage during inspiration (Figure 12.3.4). These “accessory” muscles assist the external intercostals and include the sternocleidomastoids, the scalenes, and the pectoralis minor. All of these groups allow for a greater thoracic expansion and thus a greater lung volume. Recognizing that a patient is using these muscles to breathe is a useful clinical sign; use of these muscles during rest is highly indicative of a raised respiratory effort to cope with an underlying and probably significant problem.
During forced expiration, accessory muscles of the abdomen, including the obliques, contract, forcing abdominal organs upward against the diaphragm (Figure 12.3.5). This helps to push the diaphragm further into the thorax, pushing more air out. In addition, accessory muscles (primarily the internal intercostals) help to compress the rib cage, which also reduces the volume of the thoracic cavity.
 |
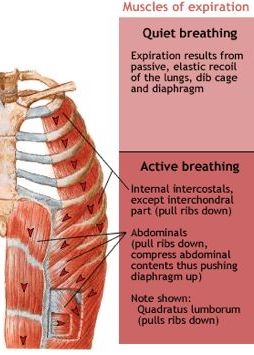 |
Resistance, Compliance, and Ventilation
Resistance
While pressure differences between the atmosphere and alveoli are the main determinants of ventilation, other factors influence the effort that must be expended to ventilate. Resistance (R) is the friction encountered by air as it passes through the airways; resistance slows the flow of gases. The greater the resistance, the greater the effort that is required to ventilate.
The diameter of the airway is the primary factor affecting resistance. A small tubular diameter forces air through a smaller space, causing more collisions of air molecules with the walls of the airways. To better understand this, consider the types of airflow that can occur in the airways. The most efficient form of flow is laminar flow; laminar flow takes the lowest pressure differential for flow to occur. In laminar flow the molecules are moving in an orderly manner, with those at the side of the tube moving a little slower due to contact with tube walls and those in the middle moving fastest (Figure 12.3.6).
When velocity increases or tube radius decreases then this organization is lost. Collisions between molecules and with the tube wall are now more frequent and movement is more chaotic, and the flow becomes turbulent (Figure 12.3.7). At this point some molecules are at times moving against the pressure gradient due to these collisions. Consequently, to generate the same amount of molecule movement (i.e., flow) from one end of the tube to another, a greater pressure differential is needed when flow becomes turbulent. Turbulent flow is more common in the large airways where velocity and airway radius are high.
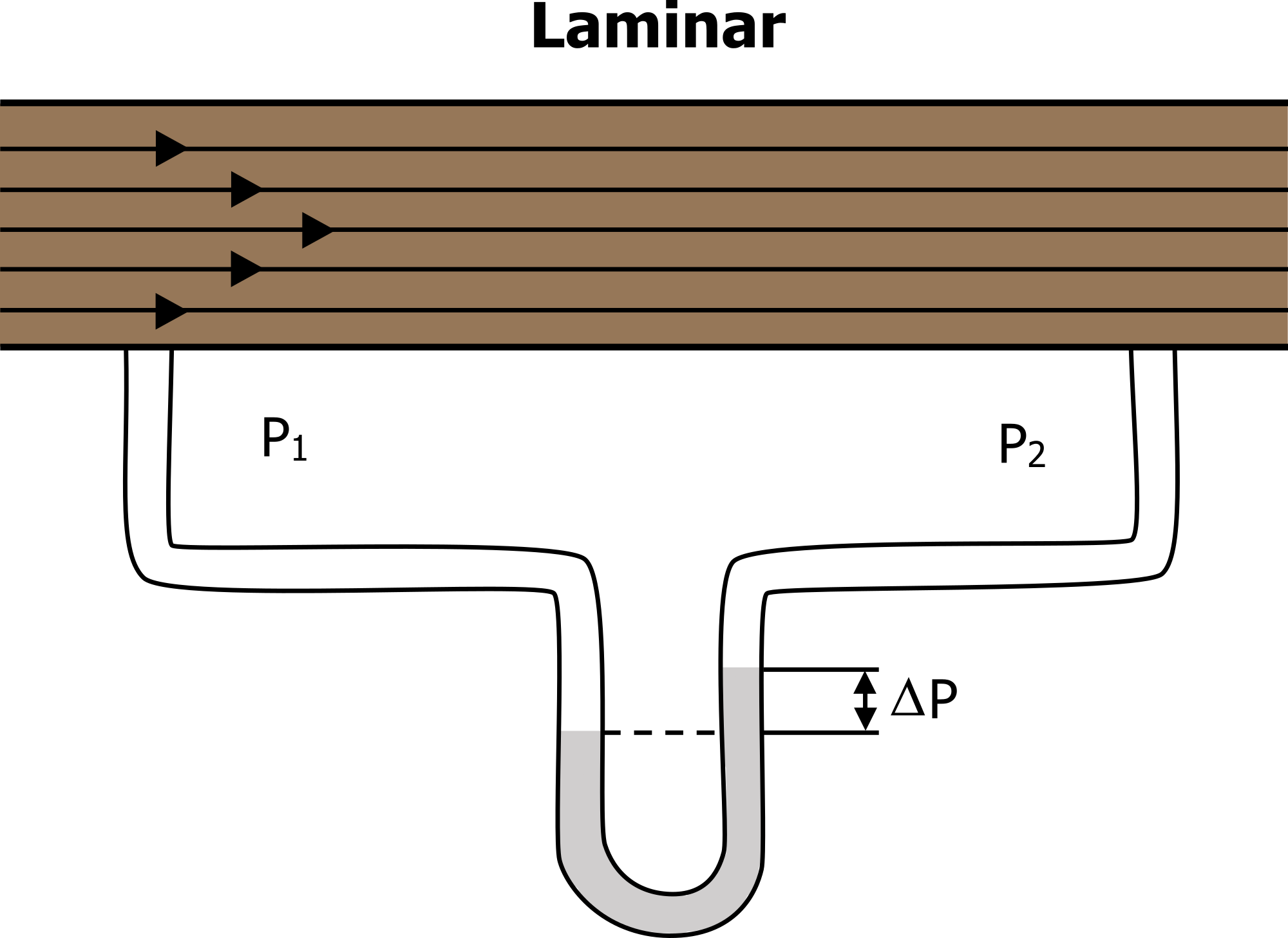 Figure 12.3.6 – Laminar Flow
Figure 12.3.6 – Laminar Flow
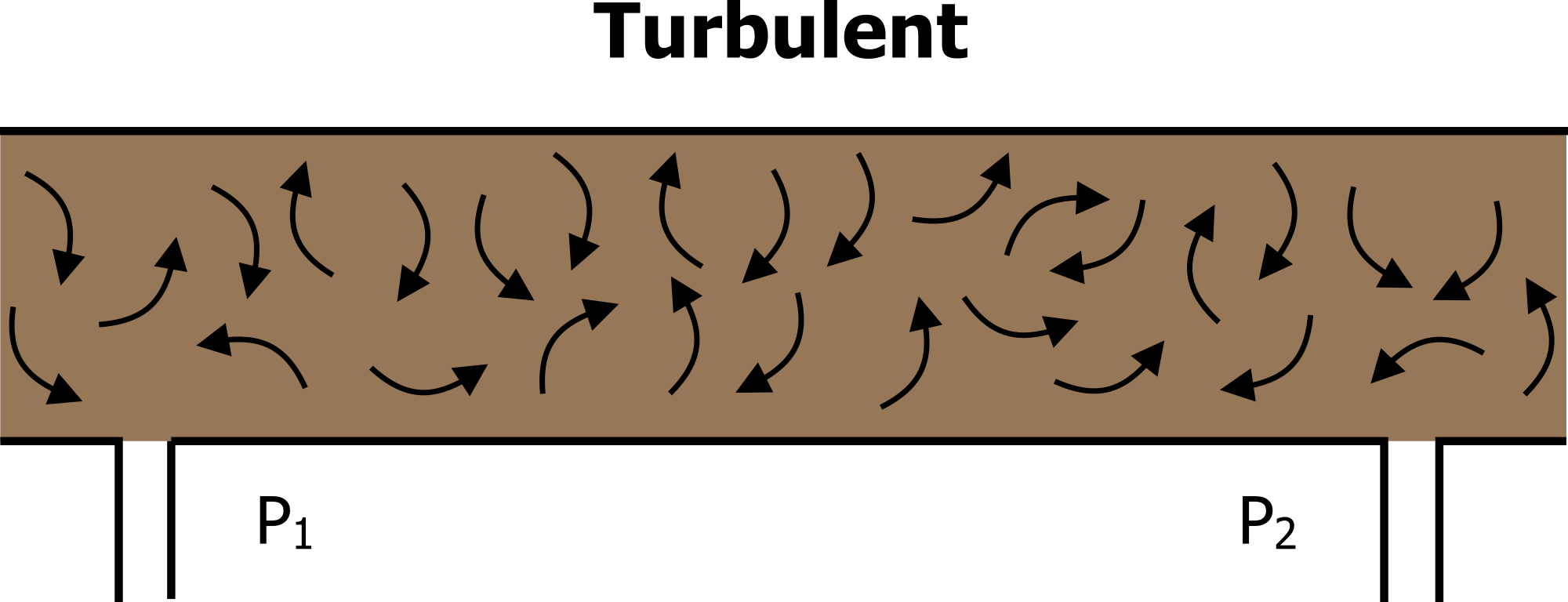 Figure 12.3.7 – Turbulent Flow
Figure 12.3.7 – Turbulent Flow
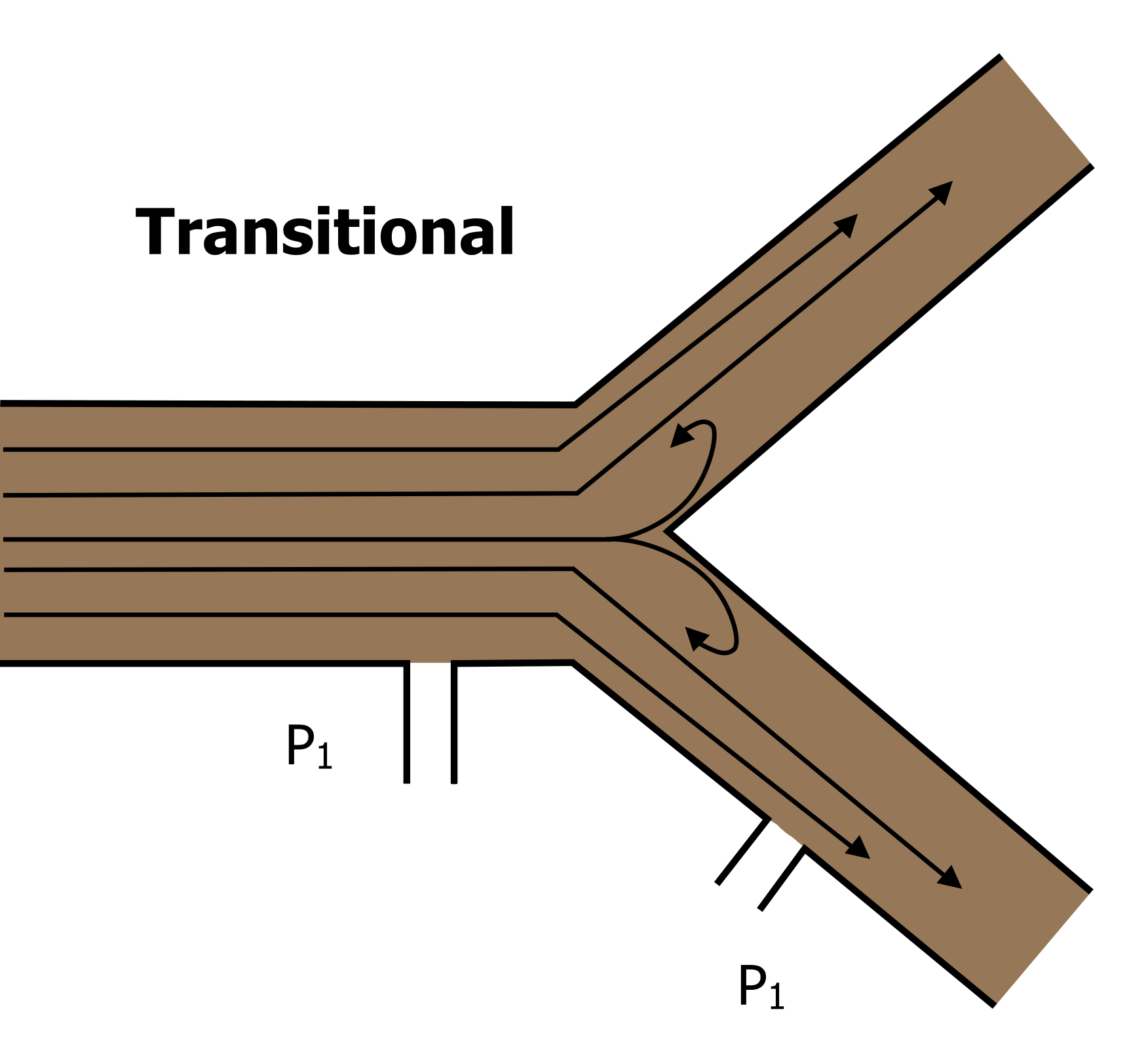
Figure 12.3.8 – Transitional Flow
In reality, the vast majority of the airways are branching small tubes, so we see a mixture of the two above—mostly laminar flow but some turbulence generated at the branch (or transitional) points (Figure 12.3.8)
The following formula helps to describe the relationship between airway resistance and pressure changes or differences between two areas in the respiratory tract:
Where: F = gas flow; ∆P = pressure difference between atmosphere and alveoli; R = resistance
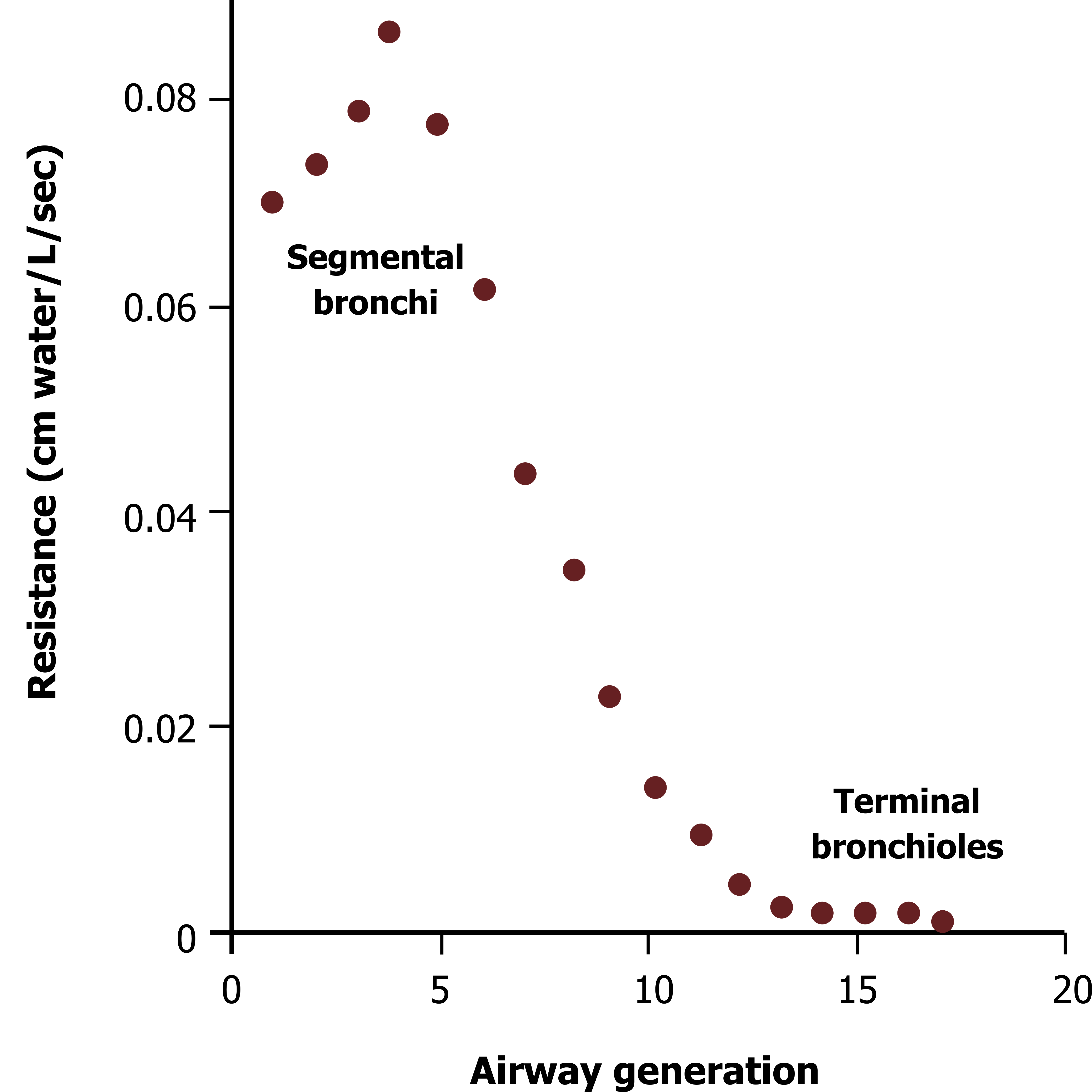 Figure 12.3.9 – Airway Resistance Down the Bronchial Tree
Figure 12.3.9 – Airway Resistance Down the Bronchial Tree
With diameter having such a powerful effect on airway resistance, we would expect that airway resistance would be a significant force to overcome during ventilation. However, in a person free of respiratory disease, airway resistance is insignificant. This is due to two main factors:
- In the first part of the conducting zone, airway diameters are huge relative to the low air viscosity.
- Although the airways get progressively smaller as we move through the bronchial tree, there are also progressively more airways; therefore despite the tiny diameters of bronchioles, there is an enormous number of them occurring in parallel which results in a large total cross-sectional area.
The greatest resistance to flow is actually in the medium-sized segmental bronchi (Figure 12.3.9).
There are a couple of clinically important points to make here:
- If radius is reduced by disease, such as during inflammation of the airway wall or contraction of airway smooth muscle causing bronchoconstriction, then resistance is markedly increased, and to maintain flow, the pressure differential must be increased. Increasing this pressure differential means increasing the work of ventilation.
- The vast total cross-sectional area of the lower airways means that a significant amount of damage can be done before symptoms arise. This “silent zone” means that a disease may be significantly established and be in a relatively late stage before the patient becomes symptomatic and goes to the physician.
Compliance
Compliance is the ability of the lungs to stretch, and therefore how easy they are to inflate. Compliance in healthy lungs is high. One factor that could make the lungs harder to inflate, i.e. less compliant, is the strong inward pull of the alveolar surface tension. However, recall that surfactant made by type II alveolar cells reduces the alveolar surface tension (see Section 12.1). In this way, surfactant production is one important factor keeping lungs compliant.
Compliance of the thoracic cavity is also important in facilitating proper ventilation. In order for inspiration to occur, the thoracic cavity must expand. The expansion of the thoracic cavity directly influences the capacity of the lungs to expand. If the tissues of the thoracic wall are not very compliant, more effort will be necessary to expand the thorax during breathing.
Respiratory Volumes and Capacities
Respiratory volumes are volumes of air moved by or associated with the lungs at a given point in the respiratory cycle. The four major respiratory volumes—tidal, expiratory reserve volume, inspiratory reserve volume, and residual volume (Figure 12.3.10)—are described further as follows:
- Tidal volume (TV) is the amount of air that normally enters or exits the lungs during quiet breathing; average TV: 500 mL.
- Expiratory reserve volume (ERV) is the amount of air you can forcefully expire past a normal tidal expiration; average ERV: 700 to 1200 mL.
- Inspiratory reserve volume (IRV) is the amount of air you can forcefully inspire past a normal tidal inspiration; average IRV: 1,900 to 3,100 mL
- Residual volume (RV) is the air left in the lungs after a forced expiration. RV is typically 1,100 to 1,200 mL. The residual volume helps keep alveoli open after expiration.
The volumes presented above are typical volumes measured in healthy individuals. Respiratory volumes are dependent upon a variety of factors, including age, sex, and body size. In general, with the exception of tidal volume, respiratory volumes tend to be smaller in females than in males due to body size differences.
Since respiratory diseases such as asthma and COPD can greatly affect respiratory volumes, measuring these volumes can provide important clues about a person’s respiratory health.
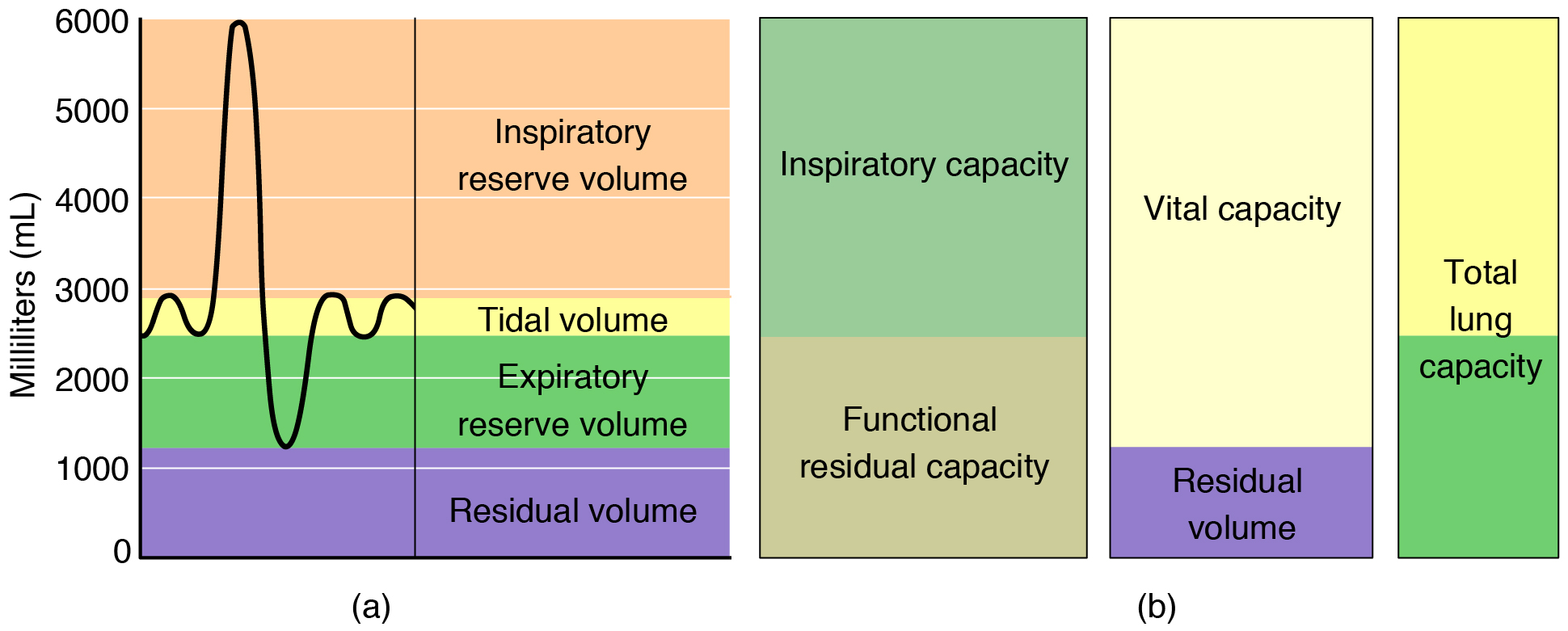
- Total lung capacity (TLC) is the sum of all of the volumes (TV + ERV + IRV + RV); TLC represents the total amount of air a person can hold in the lungs after a forceful inhalation. TLC is about 6,000 mL for males and about 4,200 mL for females.
- Vital capacity (VC) is the sum of all of the volumes except residual volume (TV + ERV + IRV); VC is the total amount of exchangeable of air (the volume of air a person can move into or out of the lungs). VC in a healthy individual is between 3,100 mL and 4,800 mL, with females typically having lower VC values.
- Inspiratory capacity (IC) is the sum of the tidal volume and inspiratory reserve volume (TV + IRV); IC is the maximum amount of air that can be inhaled past a normal tidal expiration. IC in a healthy individual is between 2,400 mL and 3,600 mL, with females typically having lower IC values.
- Functional residual capacity (FRC) is the sum of expiratory reserve volume and residual volume (ERV + RV); FRC is the amount of air that remains in the lung after a normal tidal expiration; FRC in a healthy individual is between 1,800 mL and 2,400 mL, with females typically having lower FRC values.
In addition to the air that creates respiratory volumes, the respiratory system also contains anatomical dead space, which is air that is present in the airway that never reaches the alveoli and therefore never participates in gas exchange. The anatomical dead space totals about 150 mL (see Section 12.1.) Alveolar dead space involves air found within alveoli that are unable to function, such as those affected by disease or abnormal blood flow. Total dead space is the anatomical dead space and alveolar dead space together, and represents all of the air in the respiratory system that is not being used in the gas exchange process.
Pulmonary Function Tests
Spirometry is a method used to measure respiratory volumes and capacities. Spirometry alone cannot provide a specific diagnosis but it can help evaluate losses in respiratory function and can help a clinician distinguish between categories of respiratory diseases. In addition to being used to measure certain volumes and capacities, clinicians use spirometry to assess the rate at which air flows into and out of the lungs. For example, forced vital capacity (FVC) is the volume of air expired when a person takes a deep breath and then maximally exhales as quickly as possible. Forced expiratory volume (FEV) measures the amount of air forcefully expired during certain time intervals (e.g., FEV1 is the volume of air expelled in one second).
External Website
Watch the video below to learn how a spirometry test is performed. Note that the spirometer seen in the video is just one of several types of spirometers used in hospitals and clinics. Click here to view “How to Perform a Spirometry Test” by
Clinical Connection – Respiratory Therapist
Generally speaking, respiratory therapists treat patients who are having trouble breathing. They perform a wide range of therapies, including administering oxygen, managing ventilators, and administering medications to the lungs to name just a few.
View the video below to see examples of a day in the life of a respiratory therapist. Click here to view “A Day in the Life: Respiratory Therapist | Cincinnati Children’s” by Cincinnati Children’s (April 5, 2021) in a separate tab. To access captions, click on the “cc” button in the lower right of the video after beginning the video.
Section Review
Pulmonary ventilation is the process of breathing, which is driven by pressure differences between the lungs and the atmosphere. Atmospheric pressure is the force exerted by gases present in the atmosphere. The force exerted by gases within the alveoli is called intra-alveolar (intrapulmonary) pressure, whereas the force exerted by gases in the pleural cavity is called intrapleural pressure. Typically, intrapleural pressure is lower, or negative to, intra-alveolar pressure. The difference in pressure between intrapleural and intra-alveolar pressures is called transpulmonary pressure.
Pressure is determined by the volume of the space occupied by a gas and is influenced by resistance. Air flows when a pressure gradient is created, from a space of higher pressure to a space of lower pressure. Boyle’s law describes the relationship between volume and pressure. A gas is at lower pressure in a larger volume because the gas molecules have more space to in which to move. The same quantity of gas in a smaller volume results in gas molecules crowding together, producing increased pressure.
Resistance is created by inelastic surfaces, as well as the diameters of the airways. Resistance reduces the flow of air. The surface tension of the alveoli also influences pressure, as it opposes the expansion of the alveoli. However, pulmonary surfactant helps to reduce the surface tension so that the alveoli do not collapse during expiration. The ability of the lungs to stretch, called lung compliance, also plays a role in gas flow. The more the lungs can stretch, the greater the potential volume of the lungs. The greater the volume of the lungs, the lower the air pressure within the lungs.
Pulmonary ventilation consists of the process of inspiration (or inhalation), where air enters the lungs, and expiration (or exhalation), where air leaves the lungs. During inspiration, the diaphragm and external intercostal muscles contract, causing the rib cage to expand and move outward. This expands the thoracic cavity and lung volume and creates a lower pressure within the lung than that of the atmosphere, causing air to be drawn into the lungs. During expiration, the diaphragm and intercostals relax, causing the thorax and lungs to recoil. The air pressure within the lungs increases to above atmospheric pressure, causing air to be forced out of the lungs. During forced exhalation, the internal intercostals and abdominal muscles are sometimes involved in forcing air out of the lungs.
Respiratory volume describes the amount of air in a given space within the lungs, or which can be moved by the lung, and is dependent on a variety of factors. Tidal volume refers to the amount of air that enters the lungs during quiet breathing, whereas inspiratory reserve volume is the amount of air that enters the lungs when a person inhales past the tidal volume. Expiratory reserve volume is the extra amount of air that can leave with forceful expiration, following tidal expiration. Residual volume is the amount of air that is left in the lungs after expelling the expiratory reserve volume. Respiratory capacity is the combination of two or more volumes. Anatomical dead space refers to the air within the respiratory structures that never participates in gas exchange, because it does not reach functional alveoli. Respiratory rate is the number of breaths taken per minute, which may change during certain diseases or conditions.
Review Questions
Critical Thinking Questions
Glossary
- alveolar dead space
- air space within alveoli that are unable to participate in gas exchange
- anatomical dead space
- air space present in the airway that never reaches the alveoli and therefore never participates in gas exchange
- atmospheric pressure
- amount of force that is exerted by gases in the air surrounding any given surface
-
- (lung) compliance
- ability of the lungs to stretch
- expiration
- process that causes the air to leave the lungs (also exhalation)
- expiratory reserve volume (ERV)
- amount of air that can be forcefully exhaled after a normal tidal exhalation
- functional residual capacity (FRC)
- sum of ERV and RV, which is the amount of air that remains in the lungs after a tidal expiration
- inspiration
- process that causes air to enter the lungs (also inhalation)
- inspiratory capacity (IC)
- sum of the TV and IRV, which is the amount of air that can maximally be inhaled past a tidal expiration
- inspiratory reserve volume (IRV)
- amount of air that can forcibly be inhaled past the tidal volume
- intra-alveolar pressure
- pressure of the air within the alveoli (intrapulmonary pressure)
- intrapleural pressure
- pressure within the pleural cavity
- pulmonary ventilation
- exchange of gases between the lungs and the atmosphere; breathing
- residual volume (RV)
- amount of air that remains in the lungs after maximum exhalation
- resistance
- friction encountered by air as is passes through the airways; slows air flow
- tidal volume (TV)
- amount of air that enters or exits the lungs during quiet breathing
- total dead space
- sum of the anatomical dead space and alveolar dead space
- total lung capacity (TLC)
- total amount of air that can be held in the lungs; sum of TV, ERV, IRV, and RV
- transpulmonary pressure
- pressure difference between the intrapleural and intra-alveolar pressures
- vital capacity (VC)
- sum of TV, ERV, and IRV, which is the total amount amount of exchangeable air
Glossary Flashcards
This work, Human Physiology, is adapted from Anatomy & Physiology by OpenStax, licensed under CC BY. This edition, with revised content and artwork, is licensed under CC BY-SA except where otherwise noted.
Images from Anatomy & Physiology by OpenStax are licensed under CC BY except where otherwise noted.
Access the original for free at OpenStax.
Report an Error
Did you find an error, typo, broken link, or other problem in the text? Please follow this link to the error reporting form to submit an error report to the authors.
