Chapter 13. The Urinary System
13.4 Physiology of Urine Formation: Glomerular Filtration
Learning Objectives
By the end of this section, you will be able to:
- describe glomerular filtration, including the hydrostatic and colloid osmotic forces that favor and oppose filtration;
- define glomerular filtration rate (GFR) and state a range of normal values for GFR;
- define net filtration pressure (NFP) and describe the roles of glomerular hydrostatic pressure, capsular hydrostatic pressure, and colloid osmotic (oncotic) pressure in determining NFP;
- predict specific factors that will increase or decrease GFR;
- predict the effects of specific disease states or conditions (e.g. protein malnutrition, hypotension, urinary tract obstruction) on capsular hydrostatic pressure, oncotic pressure, and/or glomerular hydrostatic pressure;
- explain the mechanisms that control renal blood flow to the glomerulus;
- predict the effect of changes in the diameter of the afferent or efferent arteriole on renal blood flow and on glomerular filtration rate (GFR);
- describe autoregulation of glomerular filtration rate (GFR) via the myogenic mechanism and list the range of mean blood pressures within which GFR is autoregulated;
- describe the tubuloglomerular feedback mechanism of controlling GFR;
- describe the main the extrinsic mechanisms for controlling GFR;
- diagram and describe the renin-angiotensin-aldosterone system (RAAS) pathway;
- describe the main factors that initiate renin release;
- describe the main physiological effects of angiotensin II; and
- explain how the regulation of systemic blood pressure by RAAS indirectly regulates GFR.
Glomerular Filtration
Glomerular filtration is a passive process: no cellular energy is used by the filtration membrane to produce filtrate. Recall that the filtration membrane lies between the blood in the glomerulus and the filtrate in the glomerular capsule: plasma is filtered through fenestrations in the capillaries and filtration slits formed by the pedicels of podocytes. Approximately 20% of your cardiac output is filtered by your kidneys per minute under resting conditions.
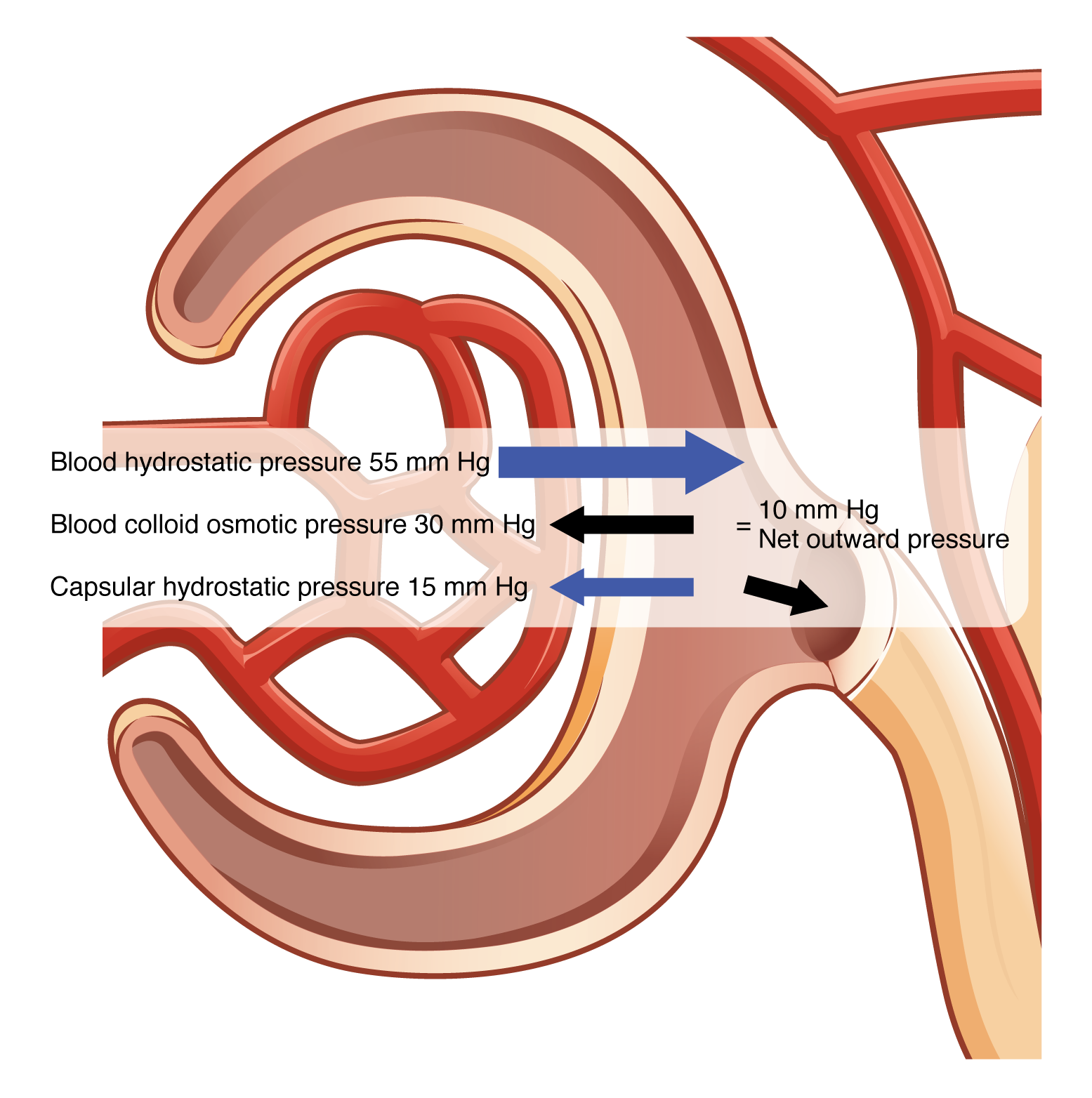
The overall force determining filtration is net filtration pressure (NFP). The value of NFP is determined by the following three forces: glomerular (blood) hydrostatic pressure, capsular hydrostatic pressure, and colloid osmotic pressure (Figure 13.4.1).
Glomerular Blood Hydrostatic Pressure, Capsular Hydrostatic Pressure, and Blood Colloid Osmotic Pressure
Hydrostatic pressure is the pressure produced by a fluid against a surface. There are two hydrostatic pressures that influence NFP at the glomerulus: glomerular blood hydrostatic pressure and capsular hydrostatic pressure. The blood inside the glomerulus creates glomerular (blood) hydrostatic pressure (GBHP) that forces fluid out of the glomerulus into the glomerular capsule. The value of GBHP is typically about 55 mm Hg. The fluid in the glomerular capsule creates pressure pushing fluid out of the glomerular capsule back into the glomerulus, thus opposing the glomerular hydrostatic pressure. This is the capsular hydrostatic pressure (CHP) and its value is approximately 15 mm Hg.
Another force opposing glomerular hydrostatic pressure is the blood colloid osmotic pressure (BCOP), or oncotic pressure, of the blood. Oncotic pressure due to plasma proteins draws fluid back into the glomerulus; its value is approximately 30 mm Hg.
In summary, glomerular blood hydrostatic pressure, which pushes fluid into the glomerular capsule, is opposed by both capsular hydrostatic pressure and blood colloid osmotic pressure.
The equation for calculating NFP is:
![]()
That is: ![]()
Or: ![]() (Figure 13.4.1).
(Figure 13.4.1).
It is important that NFP be held relatively constant because NFP directly affects the rate at which filtrate is formed, the glomerular filtration rate.
GFR (Glomerular Filtration Rate)
The volume of filtrate formed by both kidneys per minute is termed glomerular filtration rate (GFR). GFR determines how much solute is retained or discarded, how much water is retained or discarded, and ultimately, the osmolarity of blood and the blood pressure of the body:
- If GFR increases, then the rate of flow of filtrate through the nephron tubules will also increase. As a result, filtrate may be moving too quickly for substances to be reabsorbed and they will be excreted in the urine.
- If GFR decreases, then the rate of flow of filtrate through the nephron tubules will also decrease. As a result, this sluggish filtrate flow could lead to too many substances, including waste products, being reabsorbed.
Many conditions and diseases can affect NFP and therefore GFR. To read about three of these, click on each arrow below:
A normal GFR range is 90 to 125 mL filtrate formed per minute (90 to 125 mL/min). GFR is slightly lower in females compared to males, and is lower in elderly people, as GFR decreases with age. These GFR values result in about 150 to 180 L of filtrate formed per day by the kidneys. 99% of this filtrate is reabsorbed, resulting in the excretion of about 1 to 2 L of urine per day.
Regulation of GFR
Extrinsic controls are control mechanisms that originate outside of the kidney, specifically the nervous system and endocrine system. The primary function of extrinsic controls is to maintain systemic blood pressure, but in so doing, GFR is also maintained.
Intrinsic Controls: Renal Autoregulation
Recall that one force affecting NFP is glomerular blood hydrostatic pressure. If blood flow into the glomerulus increased, for example if MAP increased, then GFR could increase. Conversely, if MAP decreased, blood flow into the glomerulus would decrease, and GFR could decrease. Renal autoregulation prevents changes in GFR despite changes in systemic MAP.
The kidneys are very effective at regulating the rate of blood flow into the glomeruli over a wide range of blood pressure (MAP) values. Your blood pressure will decrease when you are relaxed or sleeping. It will increase when exercising. Yet, despite these changes, GFR will change very little. The kidney’s ability to autoregulate can maintain GFR with a MAP of as low as 80 mm Hg to as high as 180 mm Hg. This is due to two internal autoregulatory mechanisms that operate without outside influence: the myogenic mechanism and the tubuloglomerular feedback mechanism.
Myogenic Mechanism
The myogenic mechanism regulating blood flow within the kidney depends upon a characteristic shared by most smooth muscle cells of the body. When smooth muscle is stretched, it contracts; when the stretching action stops, it relaxes, restoring its resting length. This mechanism works in the afferent arteriole that supplies the glomerulus and regulates blood flow into the glomerulus.
When MAP increases, smooth muscle in the wall of the afferent arteriole is stretched. In response, the arteriolar smooth muscle contracts, resulting in constriction of the afferent arteriole. This constriction of the afferent arteriole results in little to no change in blood flow into the glomerulus despite the increase in MAP. As a result, normal NFP and GFR are maintained. Reducing the glomerular pressure also functions to protect the fragile capillaries of the glomerulus.
When MAP drops, smooth muscle in the wall of the afferent arteriole relaxes, leading to dilation of the vessel. This results in little to no change in blood flow into the glomerulus despite the decrease in MAP. As a result, normal NFP and GFR are maintained.
Tubuloglomerular Feedback
The tubuloglomerular feedback mechanism involves the juxtaglomerular (JG) cells, or granular cells, from the juxtaglomerular apparatus (JGA) and a paracrine signaling mechanism utilizing ATP and adenosine. These juxtaglomerular cells are modified smooth muscle cells lining the afferent arteriole that can contract or relax in response to the paracrine secretions released by the macula densa. This mechanism stimulates either contraction or relaxation of afferent arteriolar smooth muscle cells, which regulates blood flow to the glomerulus (Table 13.1).
Recall that the DCT is in contact with the afferent and efferent arterioles of the glomerulus. Specialized macula densa cells in this segment of the tubule respond to changes in the fluid flow rate and Na+ concentration.
As GFR increases, there is less time for NaCl to be reabsorbed in the PCT, resulting in increased osmolarity in the filtrate. The increased fluid movement more strongly deflects single nonmotile cilia on macula densa cells. This increased osmolarity of the filtrate, and the greater flow rate within the DCT, activates macula densa cells to respond by releasing ATP and adenosine (a metabolite of ATP). ATP and adenosine act locally as paracrine factors to stimulate the myogenic juxtaglomerular cells of the afferent arteriole to constrict, slowing blood flow into the glomerulus. This vasoconstriction lowers blood flow into the glomerulus, which decreases the glomerular filtration rate (GFR), correcting the initial disturbance in GFR.
Conversely, when GFR decreases, less NaCl is in the filtrate, and most will be reabsorbed before reaching the macula densa. This will result in decreased ATP and adenosine release, causing the afferent arteriole to dilate and GFR to increase. This vasodilation increases blood flow into the glomerulus, which increases the glomerular filtration rate (GFR), correcting the initial disturbance in GFR.
| Initial Change in GFR | Change in Filtrate NaCl content | Role of ATP and Adenosine/Role of NO | Effect on GFR (Corrects Initial Change) |
|---|---|---|---|
| Increased GFR | Filtrate NaCl increases | ATP and adenosine increase, causing vasoconstriction | Vasoconstriction slows GFR |
| Decreased GFR | Filtrate NaCl decreases | ATP and adenosine decrease, causing vasodilation | Vasodilation increases GFR |
Extrinsic Controls: Neural and Hormonal Mechanisms
The extrinsic control mechanisms have an effect on GFR, but their primary function is to maintain systemic blood pressure. While the intrinsic controls functioned to specifically control GFR at the level of the kidneys, the neural and hormonal controls have a broader, systemic function.
Sympathetic Influence on the Kidneys
The kidneys are innervated by the sympathetic neurons of the autonomic nervous system via the celiac plexus and splanchnic nerves. Decreased sympathetic stimulation results in vasodilation and increased blood flow through the kidneys during resting conditions. Increased sympathetic stimulation leads to vasoconstriction of arterioles serving the kidneys, ultimately resulting in slightly diminished glomerular flow.
Under conditions of stress, sympathetic nervous activity increases further, resulting in the direct vasoconstriction of afferent arterioles (norepinephrine effect) as well as stimulation of the adrenal medulla. The adrenal medulla, in turn, produces a generalized vasoconstriction through the release of epinephrine. This includes vasoconstriction of the afferent arterioles, further reducing the volume of blood flowing through the kidneys. This process redirects blood to other organs with more immediate needs. Under severe stress, such as significant blood loss, sympathetic nervous system activity increases further to keep the blood routed to essential organs and keep the body alive. The strong vasoconstriction required to maintain systemic blood pressure under these severe conditions significantly reduces blood flow to the kidneys and can be damaging to the kidney tissues.
Renin-Angiotensin-Aldosterone System (RAAS)
Recall that renin is an enzyme that is produced by the granular cells of the afferent arteriole at the JGA. It enzymatically converts angiotensinogen (made by the liver, freely circulating) into angiotensin I. The release of renin is stimulated by any of the following:
- decreased filtrate flow or decreased filtrate NaCl
- decreased stretch of granular cells
- direct sympathetic stimulation of granular cells
Angiotensin-converting enzyme (ACE) enzymatically converts inactive angiotensin I into active angiotensin II (Figure 13.4.2). ACE is not a hormone but it is functionally important in regulating systemic blood pressure and in kidney function. It is a membrane-bound enzyme found in endothelial cells lining blood vessels, mainly those in the lungs and in the kidneys. Due to its role in converting angiotensin I into angiotensin II, ACE is important in increasing blood pressure and this is why people with high blood pressure are sometimes prescribed medications called ACE inhibitors to lower their blood pressure.
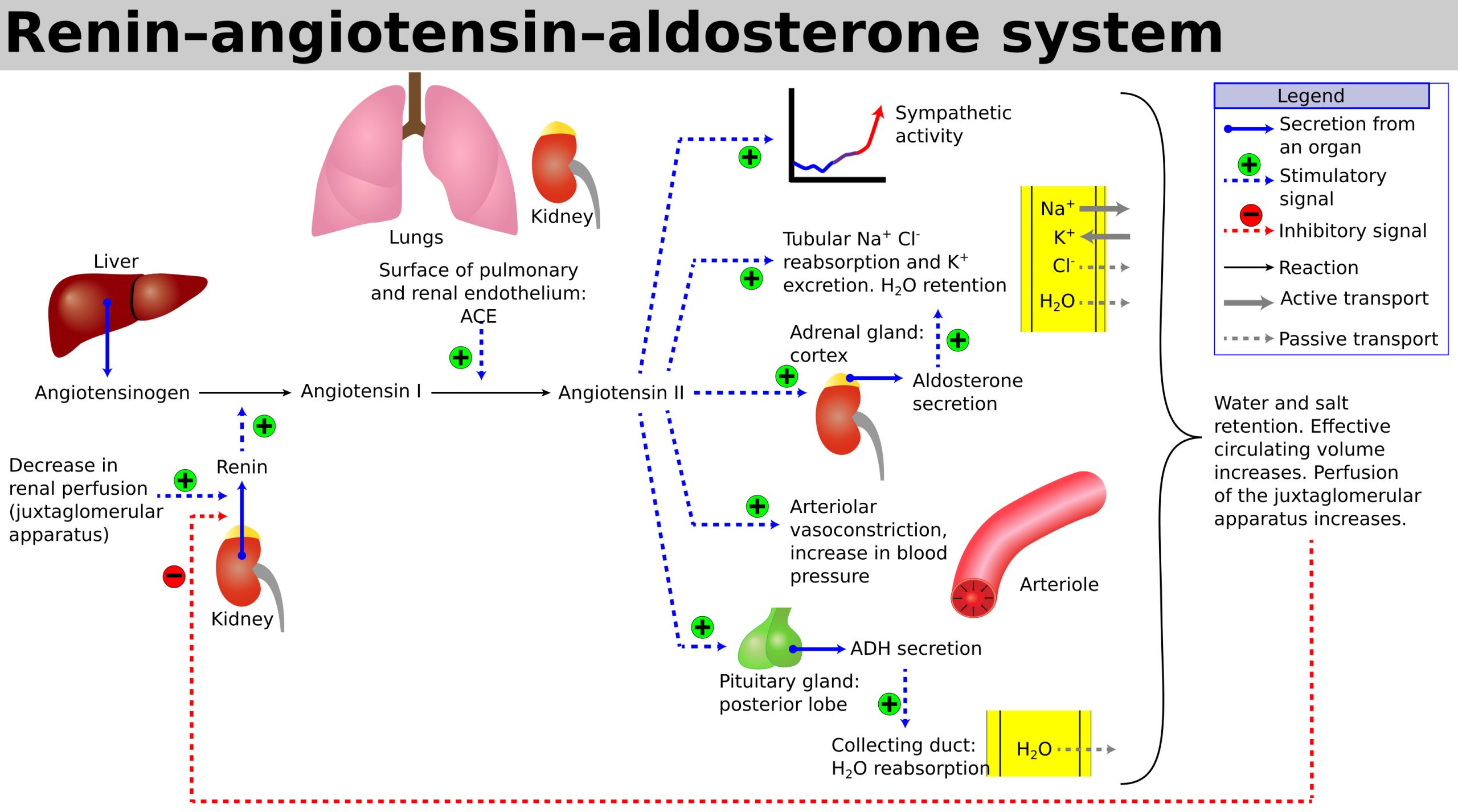
- Angiotensin II is a potent systemic vasoconstrictor that plays an immediate role in the regulation of blood pressure. Vasoconstriction increases vascular resistance (TPR), thus increasing MAP.
- Angiotensin II stimulates the release of the steroid hormone aldosterone from the adrenal cortex. Aldosterone stimulates Na+ reabsorption by the nephron, promoting the retention of water. Aldosterone is also important in regulating K+ by stimulating K+ secretion. When aldosterone levels increase, blood Na+ increases and blood K+ decreases.
- Progesterone is a steroid that is structurally similar to aldosterone. It binds to the aldosterone receptor and weakly stimulates Na+ reabsorption and increased water recovery. This process is unimportant in males due to low levels of circulating progesterone. However increased retention of water may occur at some points during the monthly reproductive cycle in females when progesterone levels increases.
- Angiotensin II stimulates the secretion of antidiuretic hormone (ADH) from the posterior pituitary gland. ADH is made in the hypothalamus and secreted by the posterior pituitary. It promotes the recovery of water, decreases urine volume, and maintains plasma osmolarity and blood pressure. (Note that angiotensin II is not the only stimulus for ADH release; this hormone is covered in more detail in an earlier chapter and later in this chapter.)
- Angiotensin II increases sympathetic nervous system activity, which would increase blood pressure.
Section Review
Net filtration pressure (NFP) is affected by three main forces: glomerular blood hydrostatic pressure, capsular hydrostatic pressure, and blood colloid osmotic pressure, or oncotic pressure. It is important that NFP remain constant, since NFP ultimately determines GFR, the glomerular filtration rate.
It is important that GFR remain constant so that the filtrate is moving at an appropropriate rate at which reabsorption can occur. Changes in GFR can result in too few of too many substances being reabsorbed.
Control of GFR occurs via intrinsic and extrinsic mechanisms. Intrinsic mechanisms are termed renal autoregulation mechanisms since these controls reside within the kidneys. Renal autoregulation regulates GFR by controlling blood flow into the glomerulus. The two mechanisms of renal autoregulation are the myogenic mechanism and tubuloglomerular feedback. Extrinsic controls of GFR occur via the sympathetic nervous system and the endocrine system. the main function of extrinsic controls is to maintain systemic blood pressure, and in doing so, GFR is maintained.
The renin-angiotensin-aldosterone system, or RAAS, is a vital regulator of systemic blood pressure in the body. Renin, secreted by the granular cells, is a hormone that has an enzymatic function; it catalyzes the conversion of angiotensinogen into angiotensin I. ACE, angiotensin-converting enzyme, converts angiotensin I into angiotensin II, which in turn has effects that increase systemic blood pressure.
Review Questions
Critical Thinking Questions
Glossary
- aldosterone
- hormone produced by the adrenal cortex; stimulates sodium reabsorption and potassium secretion by the nephron
- angiotensin converting enzyme (ACE)
- membrane-bound enzyme found in endothelial cells; it catalyzes the second step in the RAAS pathway: angiotensin I to angiotensin II
- blood colloid osmotic pressure
- “pull” of fluid into glomerulus from glomerular capsule; force due to presence of plasma proteins
- capsular hydrostatic pressure
- pressure of fluid (filtrate) in glomerular capsule pushing on the glomerulus
- glomerular blood hydrostatic pressure
- blood pressure in the glomerulus
- glomerular filtration rate (GFR)
- volume of filtrate formed per minute by the kidneys
- myogenic mechanism
- mechanism by which smooth muscle responds to stretch by contracting; an increase in blood pressure causes vasoconstriction and a decrease in blood pressure causes vasodilation so that blood flow downstream remains steady
- net filtration pressure (NFP)
- the sum pressure of fluid across the glomerulus; calculated by taking the hydrostatic pressure of the capillary and subtracting the colloid osmotic pressure of the blood and the hydrostatic pressure of the glomerular capsule
- renin
- hormone secreted by the granular (juxtaglomerular) cells; it catalyzes the first step in the RAAS pathway: angiotensinogen to angiotensin I
- tubuloglomerular feedback
- feedback mechanism involving the JGA; macula densa cells monitor Na+ concentration in the terminal portion of the ascending loop of Henle and act to cause vasoconstriction or vasodilation of afferent and efferent arterioles to alter GFR
Glossary Flashcards
This work, Human Physiology, is adapted from Anatomy & Physiology by OpenStax, licensed under CC BY. This edition, with revised content and artwork, is licensed under CC BY-SA except where otherwise noted.
Images from Anatomy & Physiology by OpenStax are licensed under CC BY except where otherwise noted.
Access the original for free at OpenStax.
Report an Error
Did you find an error, typo, broken link, or other problem in the text? Please follow this link to the error reporting form to submit an error report to the authors.
