Chapter 14. Fluid, Electrolyte, and Acid-Base Balance
14.1 Fluid Balance: Maintaining Water Balance and ECF Osmolarity
Learning Objectives
By the end of this section, you will be able to:
- list the main sources of body water intake and body water output;
- identify the main route by which water leaves the body;
- list and describe the three main stimuli that initiate the thirst response;
- explain how the thirst response restores blood osmolarity;
- describe the role of ADH (vasopressin) in maintaining water balance;
- describe the role of aldosterone in maintaining water balance;
- explain the effect of ADH (vasopressin) on blood vessel diameter; and
- define the terms diuresis and diuretic and explain how alcohol and caffeine act as diuretics.
Body Fluid Compartments (Review)
As discussed in detail in Chapter 4, body fluids occupy two main fluid compartments. The intracellular fluid (ICF) compartment includes all fluid enclosed in cells by their plasma membranes. Extracellular fluid (ECF) surrounds all cells in the body. There are two subcompartments of ECF: the plasma (liquid component of blood surrounding blood cells) and the interstitial fluid (IF) in the microscopic spaces in between tissue cells, not within blood vessels (Figure 14.1.1).
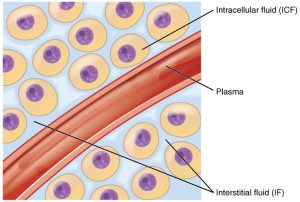
Exchanges of substances occur between the ECF and ICF across the plasma membrane, and exchanges between the plasma and interstitial fluid are made across capillary walls.
Water moves freely between all compartments, so the osmolarities of all the compartments remain equal; even if a change in osmolarity occurs in one of the fluids, eventually the osmolarities will equalize due to water movement.
If you need a review of osmolarity as a concentration measure, click on the arrows in the dropdown menus below:
While the ECF and ICF have equal osmolarities, the electrolytes in the ECF are not equal in concentration. See Figure 14.1.2 for a review.
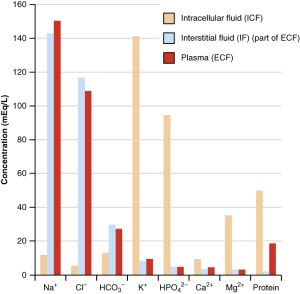
It is essential to remember that ECF osmolarity determines ICF volume. For example, if ECF osmolarity increases, the ECF osmotic pressure increases, and water will be drawn out of the cells via osmosis, causing a decrease in ICF volume. If ECF osmolarity decreases, water will move into cells via osmosis, causing an increase in ICF volume. Changes in ICF volume and osmolarity can have drastic effects on cell function, so it is vital that ECF osmolarity be maintained in order to avoid these volume shifts.
A healthy body maintains plasma osmolarity within 280 to 300 milliosmoles (mOsm) by employing several mechanisms that regulate both body water intake and output.
In order to preserve total body water content, water intake must equal water output. The major sources of water intake and output are summarized in Table 14.1.
| Average Water Intake per Day | Average Water Output per Day | ||
|---|---|---|---|
| Source of Intake | Volume (mL) | Source of Loss | Volume (mL) |
| Beverages | 1,500 | Urine | 1,500 |
| Foods | 750 | Insensible loss via lungs and skin | 700 |
| Metabolism (metabolic water) | 250 | Sweat | 200 |
| Feces | 100 | ||
| TOTAL AVERAGE INTAKE | 2,500 | TOTAL AVERAGE LOSS | 2,500 |
On a typical day, the average adult will take in about 2,500 mL of water. Although most of the intake comes through the digestive tract, about 250 mL per day is generated metabolically, in the last steps of aerobic respiration. This is called metabolic water. Additionally, each day about the same volume (2,500 mL) of water leaves the body by different routes; most of this lost water is removed as urine.
Insensible water loss is the loss of water through the skin via evaporation from the skin surface (without overt sweating) and from air expelled from the lungs. This type of loss is called “insensible” water loss because it is not easily measured and a person is usually unaware of it. All other routes of measurable water loss are examples of sensible water loss.
Regulation of Water Intake
The main force for water intake is the thirst response (Figure 14.1.3). This response is controlled by the thirst center in the hypothalamus, and it is triggered by three main stimuli:
- increased blood (ECF) osmolarity;
- dry mouth; and
- decreased blood volume leading to decreased blood pressure.
Stimulus for Thirst Response: Increased Blood Osmolarity
Osmoreceptors are sensory receptors in the thirst center in the hypothalamus that monitor the osmolarity of the blood. If blood osmolarity increases above the homeostatic range of 280 to 300 mOsm, the hypothalamus transmits signals that result in a conscious awareness of thirst. The person should (and normally does) respond by drinking water.
Stimulus for Thirst Response: Dry Mouth
In addition, when blood osmolarity increases, the salivary glands reduce saliva secretion. This change in a “dry mouth” and the sensation of thirst.
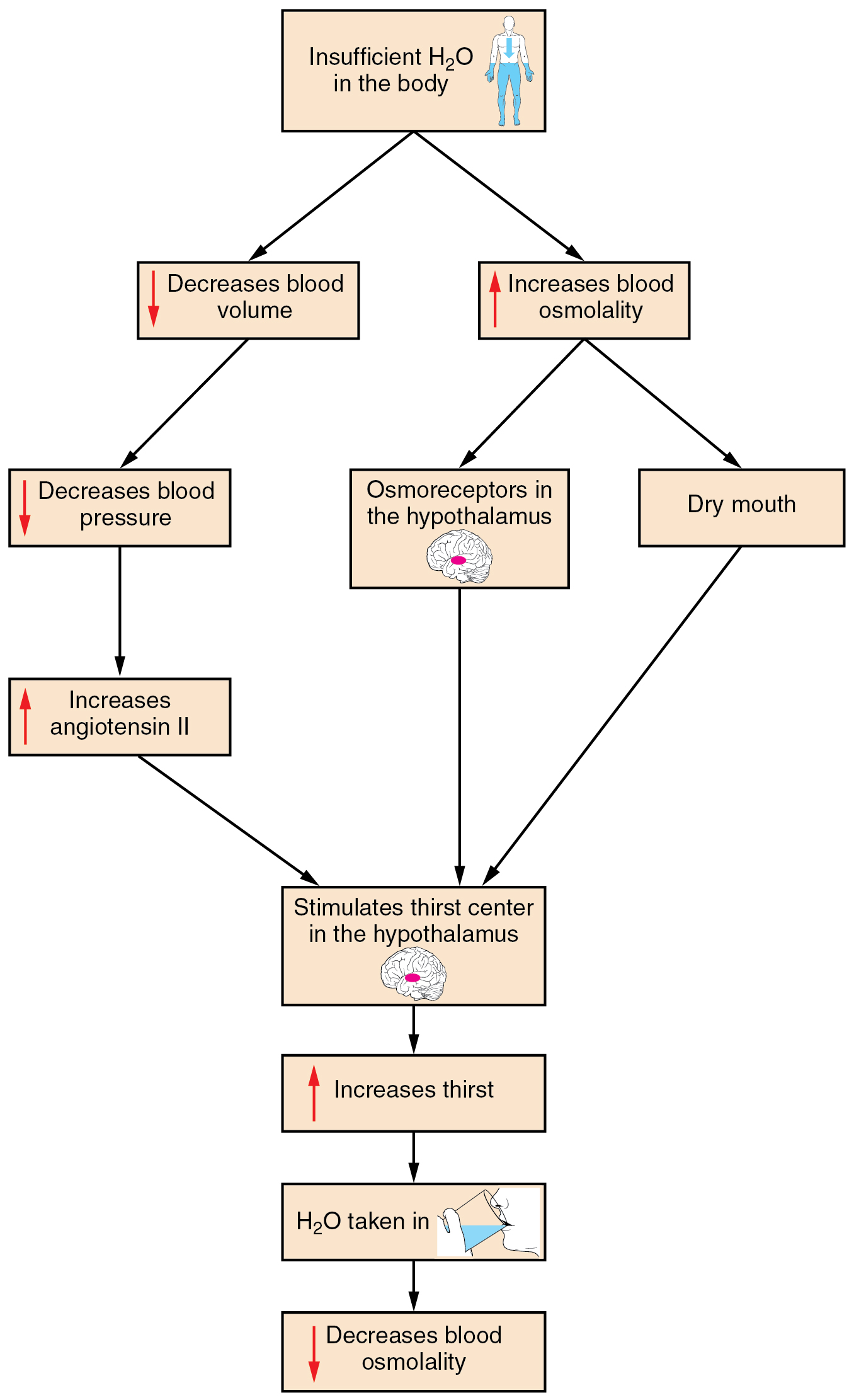
Stimulus for Thirst Response: Decreased Blood Volume and Blood Pressure
Decreased blood volume resulting from water loss has two additional effects. First, the baroreceptors in the aortic arch and in the carotid arteries detect a decrease in blood pressure that results from decreased blood volume. The heart is ultimately signaled to increase its rate and contractility to compensate for the lowered blood pressure. Second, the decreased blood pressure increases the activity of RAAS, resulting in an increase in the hormone angiotensin II, which in turn stimulates thirst (Figure 14.1.4).
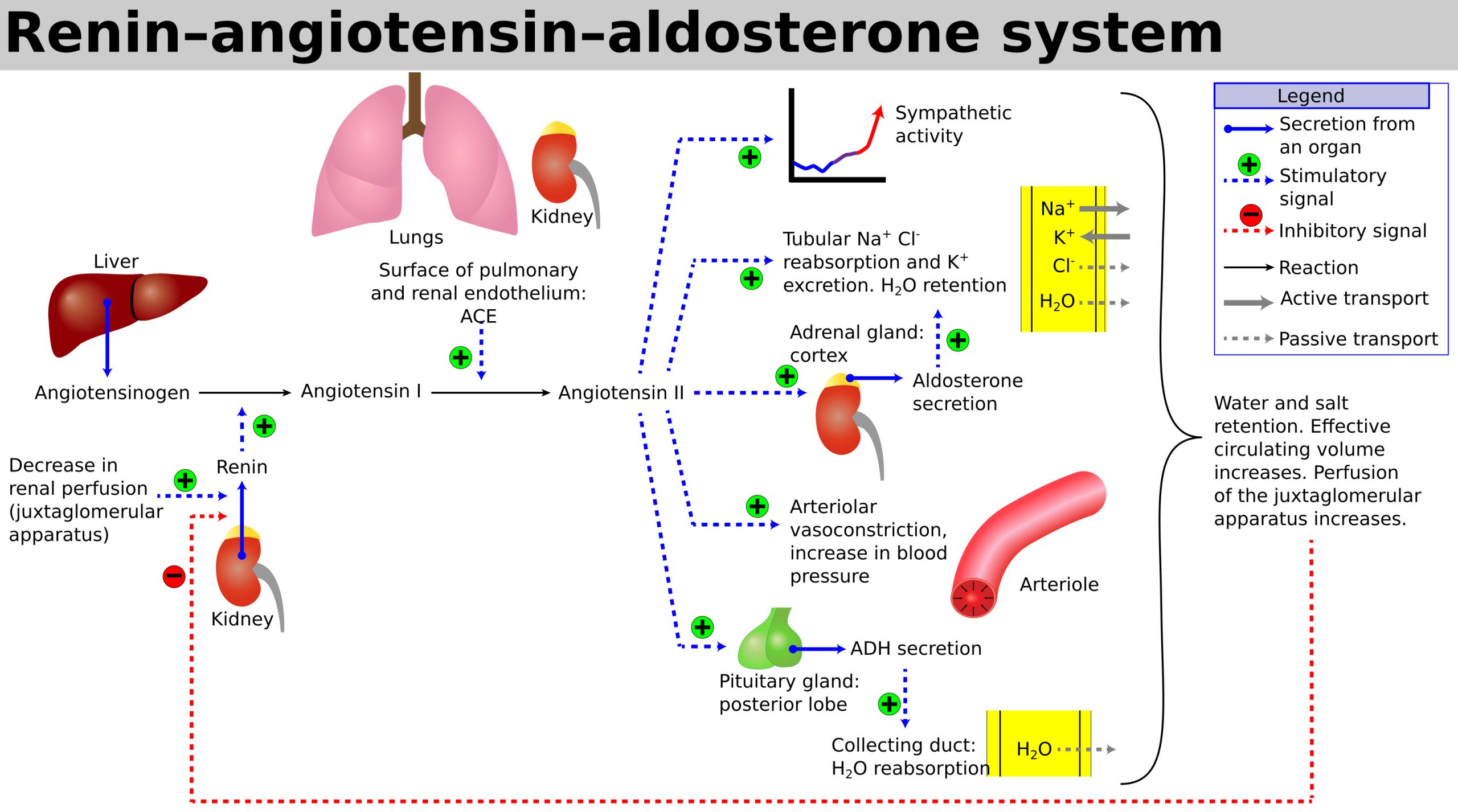
Angiotensin II also stimulates the release of the hormone aldosterone from the adrenal glands (Figure 14.1.4). Aldosterone increases the reabsorption of sodium in the distal tubules of the nephrons in the kidneys, and water follows this reabsorbed sodium back into the blood. Circulating angiotensin II also stimulates the hypothalamus to release ADH via the posterior pituitary. ADH in turn conserves water by stimulating water reabsorption by the kidneys (Figure 14.1.5).
Regulation of Water Output
Water loss from the body occurs predominantly through the renal system. A person produces an average of 1.5 L of urine per day. Although the volume of urine varies in response to hydration levels, there is a minimum volume of urine production required for proper bodily functions. The kidney excretes 100 to 1,200 mOsm of solutes per day to rid the body of a variety of excess salts and other water-soluble chemical wastes, most notably creatinine, urea, and uric acid. Failure to produce the minimum volume of urine means that metabolic wastes cannot be effectively removed from the body, a situation that can impair organ function. The minimum level of urine production necessary to maintain normal function is about 0.47 L per day.
The kidneys can regulate water levels in the body: they can conserve water and excrete concentrated urine if you are dehydrated and they can excrete dilute urine to eliminate excess water if necessary.
Role of ADH
ADH controls water loss from the body via the urine. When the osmoreceptors in the hypothalamus detect an increase in blood osmolarity, the hypothalamus signals the release of ADH from the posterior pituitary into the blood. With increased ADH, the distal convoluted tubules and collecting ducts of the nephrons become permeable to water and water is reabsorbed into the blood from the filtrate. This conserves water and prevents it from being excreted in the urine.
When blood osmolarity decreases and the level of ADH decreases, resulting in more water being excreted in the urine.
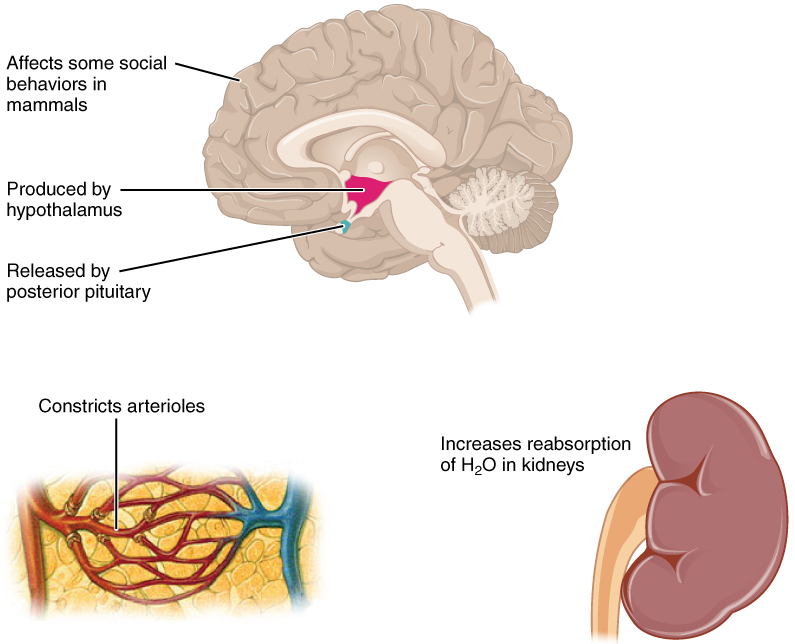
ADH is also called vasopressin due to its other main effect. At higher levels, ADH (vasopressin) causes systemic vasoconstriction (“vaso” meaning “vessel”; “pressor” meaning “pressure”). This increases blood pressure and also helps increase blood supply to the core of the body.
Water Balance Disorders
Dehydration
Dehydration is a net loss of water that results in insufficient water in blood and other tissues. If adequate fluids are not consumed, dehydration results and a person’s body contains too little water to function correctly. A person who repeatedly vomits or who has diarrhea may become dehydrated, and infants, because their body mass is so low, can become dangerously dehydrated very quickly. Endurance athletes such as distance runners can become dehydrated during long races if they do not properly hydrate during a race. Dehydration can be a medical emergency, and a dehydrated person may lose consciousness, become comatose, or die, if the body is not rehydrated quickly.
Hypotonic Hydration
Hypotonic hydration is dilution of the ECF; it is a type of overhydration. When there is renal insufficiency or we drink an extraordinary amount of water very quickly, hypotonic hydration can occur. In this condition, the ECF is diluted due to the large influx of water—the sodium content is normal, but excess water is present so the sodium concentration is low.
Hypotonic hydration can result in nausea, vomiting, muscular cramping, and cerebral edema. Cerebral edema can quickly result in disorientation, convulsions, coma, and death if left untreated.
Diuresis, which is excessive urine production, begins about 30 minutes after drinking a large quantity of fluid. Diuresis reaches a peak after about 1 hour, and normal urine production is reestablished after about 3 hours.
A diuretic is a compound that increases urine volume. Three familiar drinks contain diuretic compounds: coffee, tea, and alcohol. The caffeine in coffee and tea promotes vasodilation in the nephron, which increases GFR and leads to diuresis. Caffeine also lessens Na+ reabsorption by the PCT, resulting in less water reabsorption.
Alcohol causes diuresis by inhibiting ADH release from the posterior pituitary, resulting in less water recovery by the DCT and collecting duct.
In cases of high blood pressure, diuretics may be prescribed to reduce blood volume and, thereby, reduce blood pressure. An example of an anti-hypertensive diuretic is hydrochlorothiazide. It inhibits the Na+/ Cl– symporter in the DCT. The result is decreased reabsoprtion of Na+ into the blood leading to a loss of Na+ and water in the urine.
Osmotic diuretics promote water loss by osmosis. An example is the indigestible sugar mannitol, which is most often administered to reduce brain swelling after head injury. However, it is not the only sugar that can produce a diuretic effect. In cases of poorly controlled diabetes mellitus, glucose levels exceed the capacity of the PCT glucose symporters, resulting in glucose in the urine. The unrecovered glucose becomes a powerful osmotic diuretic. Classically, in the days before glucose could be detected in the blood and urine, clinicians identified diabetes mellitus by the three Ps: polyuria (diuresis), polydipsia (increased thirst), and polyphagia (increased hunger).
ECF Osmolarity and Na+
Na+ Concentration
Na+ Content
Na+ content refers to the total amount of Na+ in the body. Body Na+ content is an important determinant of the ECF volume and therefore blood pressure. The hormone mechanisms controlling Na+ content are RAAS and ANP, which control renal Na+ reabsorption and excretion.
| Body Na+ Content | ECF Na+ Concentration | |
| Sensors | Indirect sensing via baroreceptors | Direct sensing via osmoreceptors |
| Regulators | RAAS and ANP | ADH and thirst response |
| Homeostatic Importance | Blood volume and blood pressure | ECF osmolarity |
As seen in Table 14.2, the roles of body Na+ content and ECF Na+ concentration in maintaining homeostasis differ, and because of this is is important to distinguish between these two parameters. Nonetheless, they do overlap and their mechanisms of control are interrelated.
Section Review
Homeostasis requires that water intake and output be balanced. Most water intake comes through the digestive tract via liquids and food, and most water is lost from the body via urine.
This thirst response is the primary force for water intake, and is stimulated by increased blood osmolarity, dry mouth, and decreased blood volume/blood pressure.
The kidneys can adjust water output by varying the concentration of the urine to reflect the body’s water needs. ADH is a hormone that is crucial to regulation of water output since it regulates how much water is reabsorbed by the distal convoluted tubules and collecting ducts of nephrons. At higher concentrations, ADH causes systemic vasoconstriction, hence its alternate name of vasopressin.
Diuresis, the production of excess urine, can result from a variety of factors. Diuretics such as alcohol and caffeine are substances that cause diuresis. Prescribed diuretic medications such as hydrochlorthiazide help alleviate hypertension by reducing body fluid volume.
Review Questions
Critical Thinking Questions
Glossary
- dehydration
- state of containing insufficient water in blood and other tissues
- diuresis
- excess production of urine
- diuretic
- compound that increases urine output, leading to decreased water conservation
- hyponatremia
- low ECF sodium concentration; abnormally low blood sodium levels
- hypotonic hydration
- overhydration of the ECF
Glossary Flashcards
This work, Human Physiology, is adapted from Anatomy & Physiology by OpenStax, licensed under CC BY. This edition, with revised content and artwork, is licensed under CC BY-SA except where otherwise noted.
Images from Anatomy & Physiology by OpenStax are licensed under CC BY except where otherwise noted.
Access the original for free at OpenStax.
Report an Error
Did you find an error, typo, broken link, or other problem in the text? Please follow this link to the error reporting form to submit an error report to the authors.
