Chapter 7. The Autonomic Nervous System
7.1 Overview of the Autonomic Nervous System
Learning Objectives
By the end of this section, you will be able to:
- Explain how the ANS uses a two-neuron chain to connect the CNS to the ANS effectors
- For the parasympathetic and sympathetic division, describe the site of CNS origin, locations of ganglia, and general fiber pathways
- Differentiate between acetylcholine and norepinephrine in terms of which neurons release them, their site of action, and their receptors
The motor branch of the nervous system can be divided into two functional parts: the somatic nervous system and the autonomic nervous system. The major differences between the two systems are evident in the responses that each produces. The somatic nervous system causes contraction of skeletal muscles. The autonomic nervous system controls cardiac and smooth muscle, as well as glandular tissue. The somatic nervous system is associated with voluntary responses (though many can happen without conscious awareness, like breathing), and the autonomic nervous system is associated with involuntary responses, such as those related to homeostasis.
The autonomic nervous system regulates many of the internal organs through a balance of two aspects, or divisions. In addition to the endocrine system, the autonomic nervous system is instrumental in homeostatic mechanisms in the body. The two divisions of the autonomic nervous system are the sympathetic division and the parasympathetic division. The sympathetic system is associated with the fight-or-flight response, and parasympathetic activity is referred to by the epithet of rest and digest. Homeostasis is the balance between the two systems. At each target effector, dual innervation determines activity. For example, the heart receives connections from both the sympathetic and parasympathetic divisions. One causes heart rate to increase, whereas the other causes heart rate to decrease.
External Website

Watch Bozeman Sciene’s video [YouTube] to learn more about adrenaline and the fight-or-flight response. When someone is said to have a rush of adrenaline, the image of bungee jumpers or skydivers usually comes to mind. But adrenaline, also known as epinephrine, is an important chemical in coordinating the body’s fight-or-flight response. In this video, you look inside the physiology of the fight-or-flight response, as envisioned for a firefighter. His body’s reaction is the result of the sympathetic division of the autonomic nervous system causing system-wide changes as it prepares for extreme responses.
Pathways and Ganglia
The autonomic nervous systems operates using a two-neuron chain system. The “first” neuron is known as the preganglionic neuron, or the central neuron. Its cell body is located in the central nervous system, and it sends projections to and synapses with the “second” neuron known as the postganglionic neuron, also referred to as the ganglionic neuron. The postganglionic neuron’s cell body is located in the autonomic ganglion and it sends projections to and synapses with the effector organ or target effector. The autonomic ganglia is a term used to refer to the collection of cell bodies of the postganglionic neurons. Preganglionic neurons are lightly myelinated, and postganglionic neurons are unmyelinated.
Key Anatomical Differences
The sympathetic and parasympathetic systems differ in sites of origin, relative lengths of their fibers, and location of their ganglia. These differences are summarized in Table 7.1.
Sites of origin. Parasympathetic preganglionic neurons are craniosacral in origin meaning they arise from the brain (cranium) and the sacral spinal cord. Sympathetic preganglionic fibers are thoracolumbar in origin, meaning they arise from the thoracic and lumbar regions of the spinal cord.
Relative lengths of fibers. The parasympathetic division has long preganglionic fibers and short postganglionic fibers. While the the sympathetic division has short preganglionic fibers and long postganglionic fibers.
Location of ganglia. The majority of parasympathetic ganglia are located in or near the effector organ. Remember their postganglionic fibers are short, and thus the ganglia will be closer to the effector organ. Sympathetic ganglia are closer to the spinal cord.
| Characteristics | Parasympathetic | Sympathetic |
|---|---|---|
| Functional role | Rest and digest | Fight or flight |
| Sites of origin | Craniosacral | Thoracolumbar |
| Relative length of fibers | Long preganglionic, short postganglionic | Short preganglionic, long postganglionic |
| Location of ganglia | Near or in effector organ | Near spinal cord |
Chemical Signaling in the Autonomic Nervous System
Where an autonomic neuron connects with a target, there is a synapse. The electrical signal of the action potential causes the release of a signaling molecule, which will bind to receptor proteins on the target cell. Synapses of the autonomic system are classified as either cholinergic, meaning that acetylcholine (ACh) is released, or adrenergic, meaning that norepinephrine is released. The terms cholinergic and adrenergic refer not only to the signaling molecule that is released but also to the class of receptors that each binds.
The cholinergic system includes two classes of receptor: the nicotinic receptor and the muscarinic receptor. Both receptor types bind to ACh and cause changes in the target cell. The nicotinic receptor is a ligand-gated cation channel or an ionotropic receptor, and the muscarinic receptor is a G protein–coupled receptor. The receptors are named for, and differentiated by, other molecules that bind to them. Whereas nicotine will bind to the nicotinic receptor and muscarine will bind to the muscarinic receptor, there is no cross-reactivity between the receptors. The situation is similar to locks and keys. Imagine two locks—one for a classroom and the other for an office—that are opened by two separate keys. The classroom key will not open the office door and the office key will not open the classroom door. This is similar to the specificity of nicotine and muscarine for their receptors. However, a master key can open multiple locks, such as a master key for the Biology Department that opens both the classroom and the office doors. This is similar to ACh that binds to both types of receptors. The molecules that define these receptors are not crucial—they are simply tools for researchers to use in the laboratory. These molecules are exogenous, meaning that they are made outside of the human body, so a researcher can use them without any confounding endogenous results (results caused by the molecules produced in the body).
The adrenergic system also has two types of receptors, named the alpha (α)-adrenergic receptor and beta (β)-adrenergic receptor. Unlike cholinergic receptors, these receptor types are not classified by which drugs can bind to them. All of them are G protein–coupled receptors. There are two types of α-adrenergic receptors, termed α1, α2, and there are three types of β-adrenergic receptors, termed β1, β2, and β3. An additional aspect of the adrenergic system is that there is a second signaling molecule called epinephrine. The chemical difference between norepinephrine and epinephrine is the addition of a methyl group (CH3) in epinephrine. The prefix “nor-” actually refers to this chemical difference, in which a methyl group is missing.
The term adrenergic should remind you of the word adrenaline, which is associated with the fight-or-flight response described at the beginning of the chapter. Adrenaline and epinephrine are two names for the same molecule. The adrenal gland (from the Latin, “ad-” meaning “on top of”; “renal” meaning “kidney”) secretes adrenaline. The ending “-ine” refers to the chemical being derived, or extracted, from the adrenal gland. A similar construction from Greek instead of Latin results in the word epinephrine (“epi-” meaning “above”; “nephr-” meaning “kidney”). In scientific usage, epinephrine is preferred in the United States, whereas adrenaline is preferred in Great Britain, because “adrenalin” was once a registered, proprietary drug name in the United States. Though the drug is no longer sold, the convention of referring to this molecule by the two different names persists. Similarly, norepinephrine and noradrenaline are two names for the same molecule.
Having understood the cholinergic and adrenergic systems, their role in the autonomic system is relatively simple to understand. All preganglionic fibers, both sympathetic and parasympathetic, release ACh. All ganglionic neurons—the targets of these preganglionic fibers (the postganglionic neurons)—have nicotinic receptors in their cell membranes. The nicotinic receptor is a ligand-gated cation channel that results in depolarization of the postsynaptic membrane. The postganglionic parasympathetic fibers also release ACh, but the receptors on their targets are muscarinic receptors, which are G protein–coupled receptors and do not exclusively cause depolarization of the postsynaptic membrane. Postganglionic sympathetic fibers release norepinephrine, except for fibers that project to sweat glands and to blood vessels associated with skeletal muscles, which release ACh (Table 7.2).
| Neuron | Parasympathetic | Sympathetic |
|---|---|---|
| Preganglionic | Acetylcholine → nicotinic receptor | Acetylcholine → nicotinic receptor |
| Postganglionic |
Acetylcholine → muscarinic receptor
|
Norepinephrine → α- or β-adrenergic receptors
Acetylcholine → muscarinic receptor (associated with sweat glands and the blood vessels associated with skeletal muscles only)
|
Signaling molecules can belong to two broad groups. Neurotransmitters are released at synapses, whereas hormones are released into the bloodstream. These are simplistic definitions, but they can help to clarify this point. Acetylcholine can be considered a neurotransmitter because it is released by axons at synapses. The adrenergic system, however, presents a challenge. Postganglionic sympathetic fibers release norepinephrine, which can be considered a neurotransmitter. But the adrenal medulla releases epinephrine and norepinephrine into circulation, so they should be considered hormones.
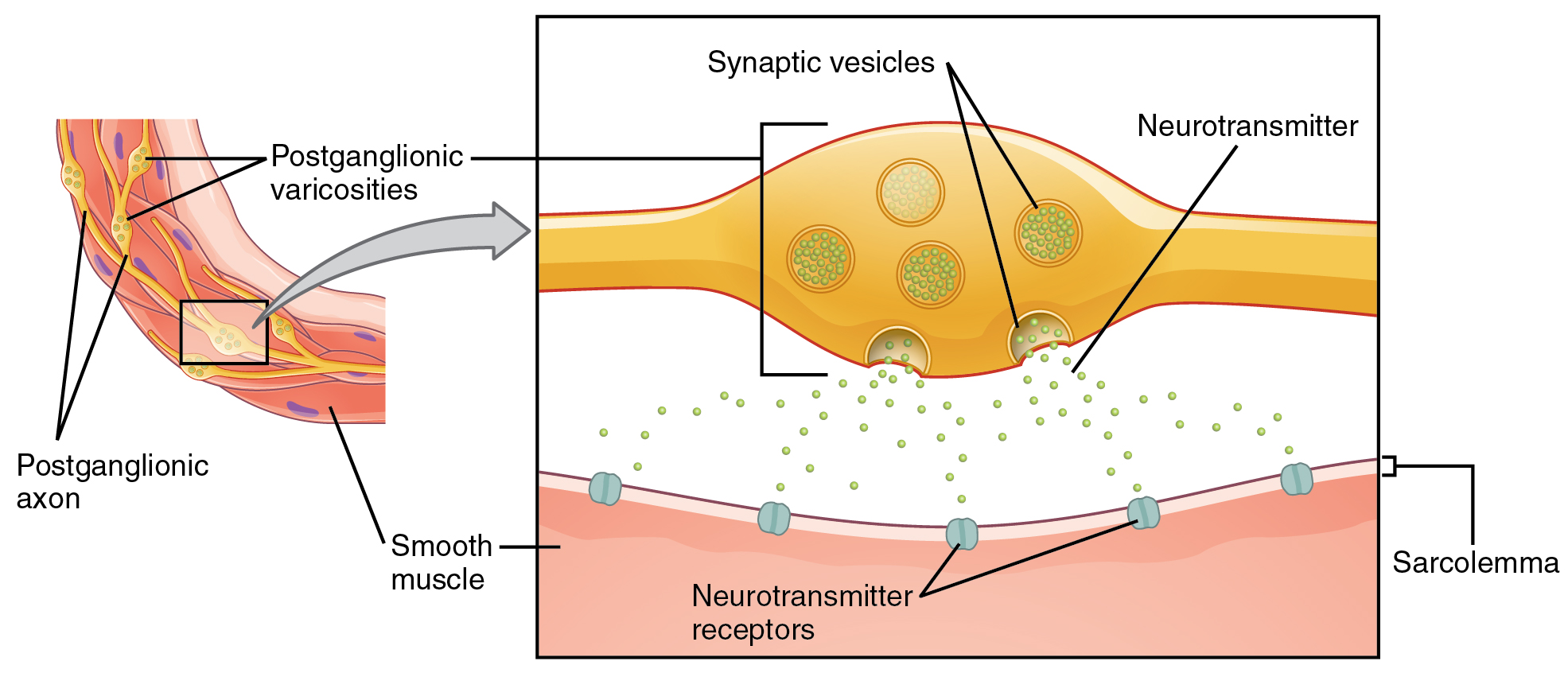
What are referred to here as synapses may not fit the strictest definition of synapse. Some sources will refer to the connection between a postganglionic fiber and a target effector as neuroeffector junctions; neurotransmitters, as defined above, would be called neuromodulators. The structure of postganglionic connections are not the typical synaptic end bulb that is found at the neuromuscular junction but rather are chains of swellings along the length of a postganglionic fiber called a varicosity (Figure 7.1.1).
Section Review
The primary responsibilities of the autonomic nervous system are to regulate homeostatic mechanisms in the body, which is also part of what the endocrine system does. The key to understanding the autonomic system is to explore the response pathways—the output of the nervous system. The way we respond to the world around us, to manage the internal environment on the basis of the external environment, is divided between two parts of the autonomic nervous system. The sympathetic division responds to threats and produces a readiness to confront the threat or to run away: the fight-or-flight response. The parasympathetic division plays the opposite role. When the external environment does not present any immediate danger, a restful mode descends on the body, and the digestive system is more active.
The autonomic nervous systems operates using a two-neuron chain system. The preganglionic neuron’s cell body is located in the central nervous and it sends projections to and synapses with the postganglionic neuron, whose cell body is located in the autonomic ganglion and it sends projections to and synapses with the effector organ. The sympathetic and parasympathetic systems differ in sites of origin, relative lengths of their fibers, and location of their ganglia. The parasympathetic division has preganglionic neurons that are craniosacral in origin, long preganglionic fibers and short postganglionic fibers, and the majority of the ganglia are located in or near the effector organ. The sympathetic division has preganglionic fibers are thoracolumbar in origin, short preganglionic fibers and long postganglionic fibers, and ganglia are closer to the spinal cord
Signaling molecules utilized by the autonomic nervous system are released from axons and can be considered as either neurotransmitters (when they directly interact with the effector) or as hormones (when they are released into the bloodstream). The same molecule, such as norepinephrine, could be considered either a neurotransmitter or a hormone on the basis of whether it is released from a postganglionic sympathetic axon or from the adrenal gland. The synapses in the autonomic system are not always the typical type of connection first described in the neuromuscular junction. Instead of having synaptic end bulbs at the very end of an axonal fiber, they may have swellings—called varicosities—along the length of a fiber so that it makes a network of connections within the target tissue.
The parasympathetic preganglionic fibers release ACh onto nicotinic receptors to excite the postganglionic neurons. The postganglionic fibers then contact the target tissues within the organ to release ACh, which binds to muscarinic receptors to induce rest-and-digest responses.
Thes sympathetic preganglionic fibers release ACh, which excites the postganglionic neuron through the nicotinic receptor. The axon from the postganglionic neuron—the postganglionic fiber—then projects to a target effector where it will release norepinephrine to bind to an adrenergic receptor, causing a change in the physiology of that organ in keeping with the broad, divergent sympathetic response. The postganglionic connections to sweat glands in the skin and blood vessels supplying skeletal muscle are, however, exceptions; those fibers release ACh onto muscarinic receptors
Review Questions
Critical Thinking Questions
Glossary
alpha (α)-adrenergic receptor
one of the receptors to which epinephrine and norepinephrine bind, which comes in two subtypes: α1 and α2
acetylcholine (ACh)
neurotransmitter that released by all preganglionic neurons
adrenergic
synapse where norepinephrine is released, which binds to α- or β-adrenergic receptors
beta (β)-adrenergic receptor
one of the receptors to which epinephrine and norepinephrine bind, which comes in two subtypes: β1 and β2
cholinergic
synapse at which acetylcholine is released and binds to the nicotinic or muscarinic receptor
endogenous
describes substance made in the human body
epinephrine
signaling molecule released from the adrenal medulla into the bloodstream as part of the sympathetic response
exogenous
describes substance made outside of the human body
G protein–coupled receptor
membrane protein complex that consists of a receptor protein that binds to a signaling molecule—a G protein—that is activated by that binding and in turn activates an effector protein (enzyme) that creates a second-messenger molecule in the cytoplasm of the target cell
ligand-gated cation channel
ion channel, such as the nicotinic receptor, that is specific to positively charged ions and opens when a molecule such as a neurotransmitter binds to it
muscarinic receptor
type of acetylcholine receptor protein that is characterized by also binding to muscarine and is a metabotropic receptor
nicotinic receptor
type of acetylcholine receptor protein that is characterized by also binding to nicotine and is an ionotropic receptor
norepinephrine
signaling molecule released as a neurotransmitter by most postganglionic sympathetic fibers as part of the sympathetic response or as a hormone into the bloodstream from the adrenal medulla
parasympathetic division
division of the autonomic nervous system responsible for restful and digestive functions
postganglionic neuron
neuron in the autonomic nervous system that projects to and synapses with the target effector
preganglionic fiber
neuron in the autonomic nervous system that projects to and synapses with a postganglionic neuron; its cell body is located in the central nervous system
sympathetic division
division of the autonomic nervous system associated with the fight-or-flight response
target effector
organ, tissue, or gland that will respond to the control of an autonomic or somatic or endocrine signal
varicosity
structure of some autonomic connections that is not a typical synaptic end bulb but rather a string of swellings along the length of a fiber that makes a network of connections with the target effector
Glossary Flashcards
This work, Human Physiology, is adapted from Anatomy & Physiology by OpenStax under CC BY. This edition, with revised content and artwork, is licensed under CC BY-SA except where otherwise noted.
Images from Anatomy & Physiology by OpenStax are licensed under CC BY except where otherwise noted.
Access the original for free at OpenStax.
Image Descriptions
Figure 7.1.1. This is a two-panel anatomical diagram illustrating the autonomic nervous system’s connection to smooth muscle. The left panel shows an overview of postganglionic axons with varicosities (bulges along the nerve fiber) extending to smooth muscle tissue. The right panel provides a magnified cross-section view showing the synaptic mechanism. In this detailed view, a yellow postganglionic nerve terminal contains multiple synaptic vesicles (circular structures) filled with neurotransmitter molecules (shown as small green dots). Some vesicles are releasing their contents into the synaptic space. Below, the pink smooth muscle tissue (sarcolemma) has neurotransmitter receptors (shown as blue circular structures) embedded in its membrane where the released neurotransmitters can bind. This diagram illustrates how nerve signals are chemically transmitted to smooth muscle to trigger contraction. [Return to Figure 7.1.1]
Report an Error
Did you find an error, typo, broken link, or other problem in the text? Please follow this link to the error reporting form to submit an error report to the authors.
