Chapter 7. The Autonomic Nervous System
7.2 Divisions of the Autonomic Nervous System
Learning Objectives
By the end of this section, you will be able to:
- Name the components that generate the sympathetic and parasympathetic responses of the autonomic nervous system
- Explain the differences in output connections within the two divisions of the autonomic nervous system
- State the effects of the parasympathetic and sympathetic divisions on their effector organs
- Recall the location and effect of binding of adrenergic receptors
- Compare and contrast the antagonistic and cooperative effects of the two branches of the autonomic nervous system
Parasympathetic Division of the Autonomic Nervous System
The parasympathetic division of the autonomic nervous system is named because its preganglionic neurons are located on either side of the thoracolumbar region of the spinal cord (“para-” meaning “beside” or “near”). The parasympathetic system can also be referred to as the craniosacral system (or outflow) because the preganglionic neurons are located in nuclei of the brainstem and the lateral horn of the sacral spinal cord.
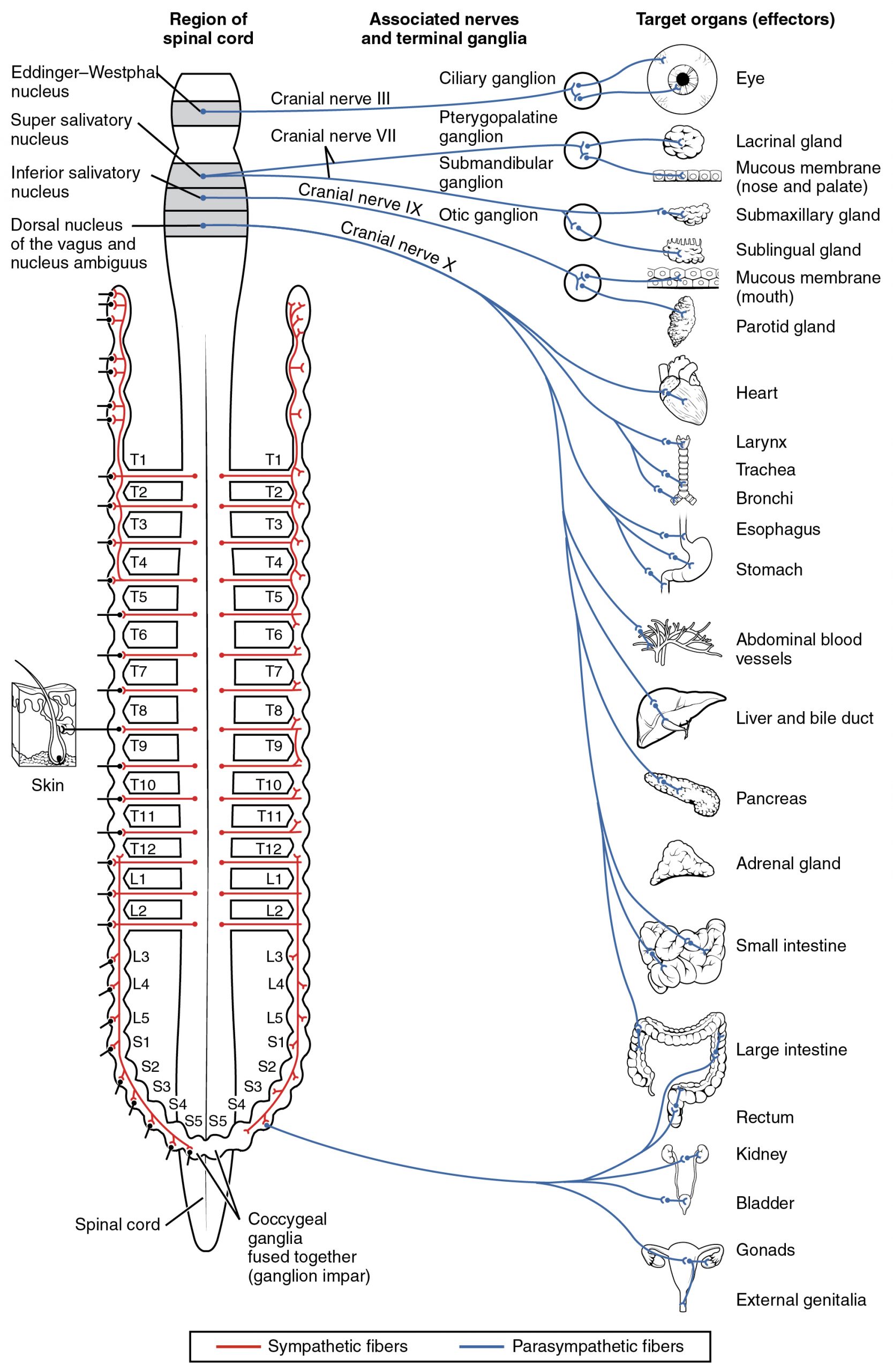
The preganglionic fibers from the cranial region travel in cranial nerves, whereas preganglionic fibers from the sacral region travel in spinal nerves. The targets of these fibers are terminal ganglia, which are located near—or even within—the target effector. These ganglia are often referred to as intramural ganglia when they are found within the walls of the target organ. The postganglionic fiber projects from the terminal ganglia a short distance to the target effector or to the specific target tissue within the organ. Comparing the relative lengths of axons in the parasympathetic system, the preganglionic fibers are long and the postganglionic fibers are short because the ganglia are close to—and sometimes within—the target effectors (Figure 7.2.1).
The cranial component of the parasympathetic system is based in particular nuclei of the brain stem. For example, in the midbrain, the Edinger–Westphal nucleus is part of the oculomotor complex, and axons from those neurons travel with the fibers in the oculomotor nerve (cranial nerve III) that innervate the extraocular muscles. The preganglionic parasympathetic fibers within cranial nerve III terminate in the ciliary ganglion, which is located in the posterior orbit. The postganglionic parasympathetic fibers then project to the smooth muscle of the iris to control pupillary size.
Sympathetic Division of the Autonomic Nervous System
To respond to a threat—to fight or to run away—the sympathetic system causes divergent effects as many different effector organs are activated together for a common purpose. More oxygen needs to be inhaled and delivered to skeletal muscle. The respiratory, cardiovascular, and musculoskeletal systems are all activated together. Additionally, sweating keeps the excess heat that comes from muscle contraction from causing the body to overheat. The digestive system shuts down so that blood is not absorbing nutrients when it should be delivering oxygen to skeletal muscles.
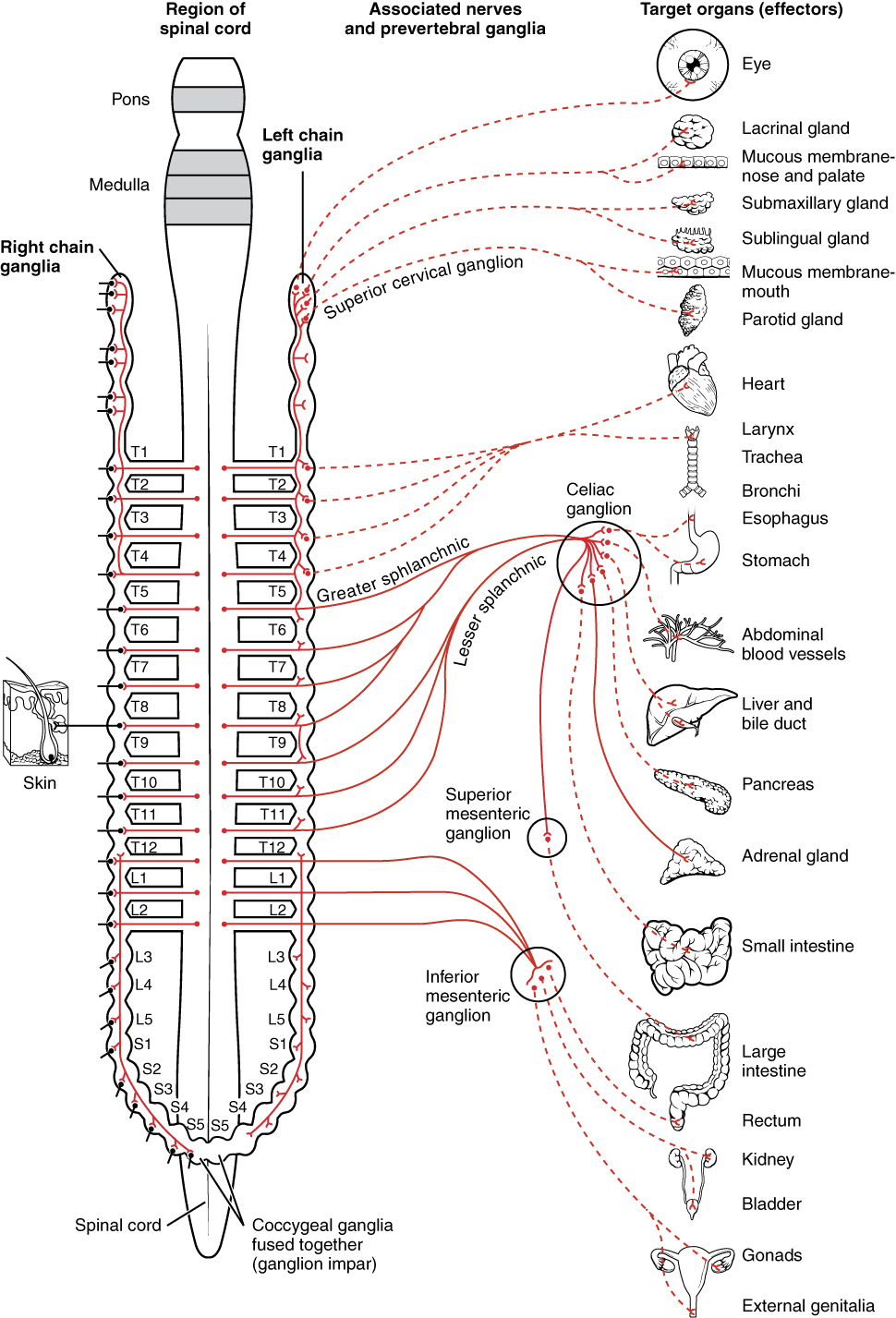
The sympathetic division of the autonomic nervous system influences the various organ systems of the body through connections emerging from the thoracic and upper lumbar spinal cord. A preganglionic in the lateral horn of any of these spinal regions projects to ganglia adjacent to the vertebral column through the ventral spinal roots. The majority of ganglia of the sympathetic system belong to a network of sympathetic chain ganglia (also known as paravertebral ganglia) that runs alongside the vertebral column. The ganglia appear as a series of clusters of neurons linked by axonal bridges. There are typically 23 ganglia in the chain on either side of the spinal column. Three correspond to the cervical region, 12 are in the thoracic region, four are in the lumbar region, and four correspond to the sacral region. The cervical and sacral levels are not connected to the spinal cord directly through the spinal roots but through ascending or descending connections through the bridges within the chain.
A diagram that shows the connections of the sympathetic system is somewhat like a circuit diagram that shows the electrical connections between different receptacles and devices. In Figure 7.2.2, the “circuits” of the sympathetic system are intentionally simplified.
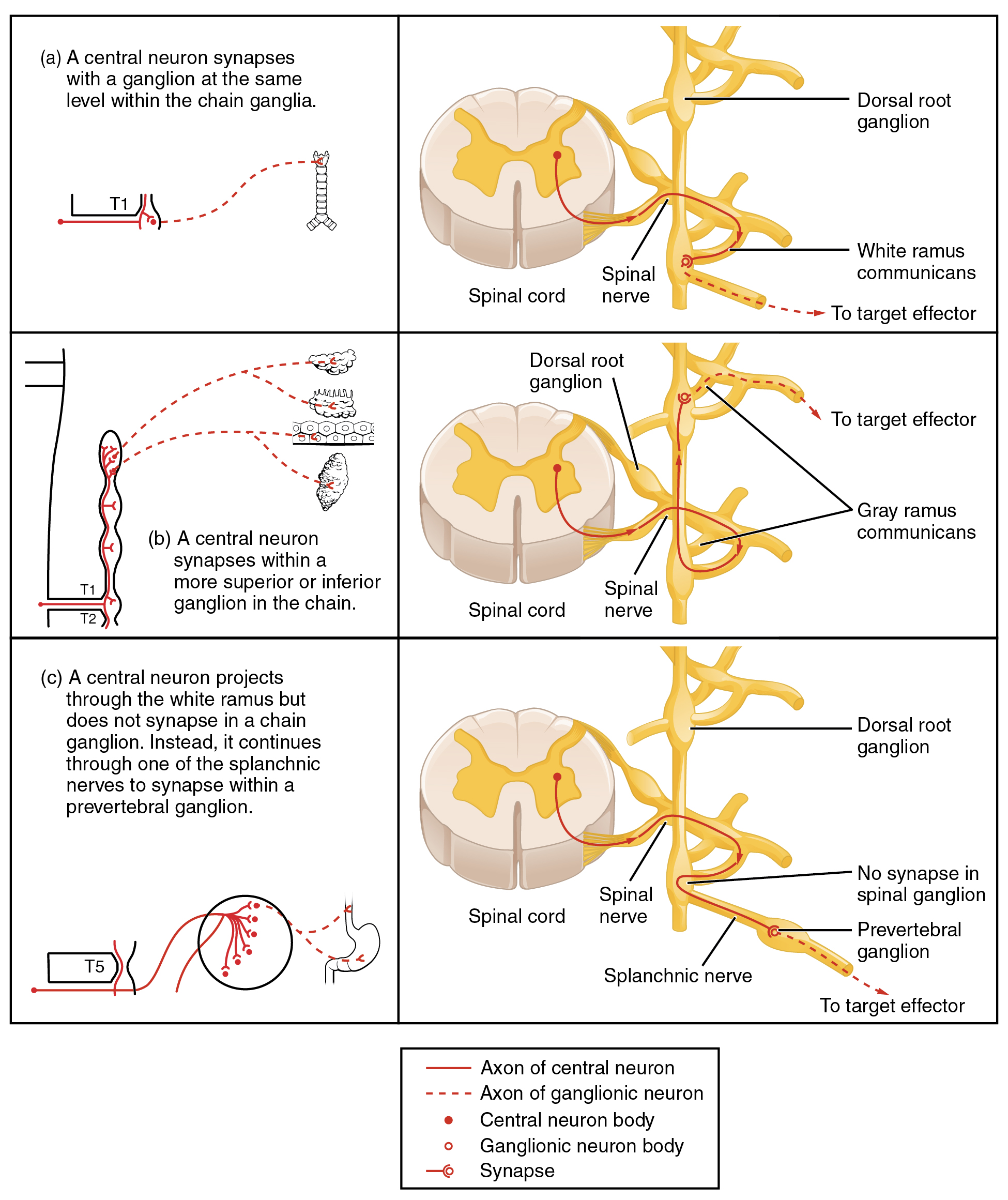
The cell bodies of the preganglionic neurons reside in the lateral horn and leave the cord via the ventral root. The neurons can then synapse on the sympathetic chain ganglia (also known as paravertebral ganglia) or the collateral ganglia (also known as prevertebral ganglia). The paravertebral ganglia are on either side of the vertebral column. The prevertebral ganglia are anterior to the vertebral column. The synapses with the trunk ganglia can occur at the same level or at higher or lower level. This means there are three different types of “junctions” that operate within the sympathetic system, meaning the synapses between the pre- and postganglionic neurons can occur at three different locations (Figure 7.2.3). The neurons can synapse at the same level, at a higher or lower level, or in a collateral ganglion.
The fibers which synapse with the chain are known as the white rami communicantes (singular ramus communicans); they are mostly myelinated and therefore referred to as white. The postganglionic neurons exit via branches or fibers known as the gray rami communicantes, which are unmyelinated axons, and continue to their effectors. As mentioned, there are two types: ones that synapse at the same level and ones that synapse at higher or lower level.
The first type is most direct: the sympathetic nerve projects to the chain ganglion at the same level as the target effector (Figure 7.2.3a). An example of this type is spinal nerve T1 that synapses with the T1 chain ganglion to innervate the trachea. The axon from the preganglionic neuron (the preganglionic fiber shown as a solid line) synapses with the postganglionic neuron (with the postganglionic fiber shown as a dashed line). This neuron then projects to a target effector—in this case, the trachea.
In the second type, the target effectors are located superior or inferior to the spinal segment at which the preganglionic fiber emerges. With respect to the “wiring” involved, the synapse with the postganglionic neuron occurs at chain ganglia superior or inferior to the location of the preganglionic neuron. An example of this is spinal nerve T1 that innervates the eye. The spinal nerve tracks up through the chain until it reaches the superior cervical ganglion, where it synapses with the postganglionic neuron (Figure 7.2.3b).
Lastly, not all axons from the preganglionic neurons terminate in the chain ganglia. Additional branches from the ventral nerve root continue through the chain and on to one of the collateral ganglia as the splanchnic nerves, including the greater splanchnic nerve, lesser splanchnic nerve, and least splanchnic nerve. For example, the greater splanchnic nerve at the level of T5 synapses with a collateral ganglion outside the chain before making the connection to the postganglionic nerves that innervate the stomach (Figure 7.2.3c).
Collateral ganglia are situated anterior to the vertebral column and receive inputs from splanchnic nerves as well as preganglionic sympathetic neurons. They are associated with controlling organs in the abdominal cavity and are also considered part of the enteric nervous system. The three collateral ganglia are the celiac ganglion, the superior mesenteric ganglion, and the inferior mesenteric ganglion (Figure 7.2.3). The word celiac is derived from the Latin word “coelom,” which refers to a body cavity (in this case, the abdominal cavity), and the word mesenteric refers to the digestive system.
One type of preganglionic sympathetic fiber does not terminate in a ganglion. These are the axons from preganglionic sympathetic neurons that project to the adrenal medulla, the interior portion of the adrenal gland. These axons are still referred to as preganglionic fibers, but the target is not a ganglion. The adrenal medulla releases signaling molecules into the bloodstream, rather than using axons to communicate with target structures. The cells in the adrenal medulla that are contacted by the preganglionic fibers are called chromaffin cells. These cells are neurosecretory cells that develop from the neural crest along with the sympathetic ganglia, reinforcing the idea that the gland is, functionally, a sympathetic ganglion.
The projections of the sympathetic division of the autonomic nervous system diverge widely, resulting in a broad influence of the system throughout the body. As a response to a threat, the sympathetic system would increase heart rate and breathing rate, increase blood flow to the skeletal muscle, and decrease blood flow to the digestive system. Sweat gland secretion should also increase as part of an integrated response. All of those physiological changes are going to be required to occur together to run away from the hunting lioness—or the modern equivalent.
The sympathetic preganglionic fibers release ACh, which excites the ganglionic neuron through the nicotinic receptor. The axon from the ganglionic neuron—the postganglionic fiber—then projects to a target effector where it will release norepinephrine to bind to an adrenergic receptor, causing a change in the physiology of that organ in keeping with the broad, divergent sympathetic response. As you might recall, there are two types of α-adrenergic receptors, termed α1, α2, and there are three types of β-adrenergic receptors, termed β1, β2, and β3. The receptor expressed depends on the organ. See Table 7.3 for a summary. The postganglionic connections to sweat glands in the skin and blood vessels supplying skeletal muscle are, however, exceptions; those fibers release ACh onto muscarinic receptors.
| Receptor Type | Major Locations | Actions |
|---|---|---|
| α1 | Blood vessels that innervate the skin, sphincters of the GI system. Smooth muscle in uterus, iris dilator muscle, and seminal tract | Vasoconstriction and decreased blood flow to affected organs, pyloric and urinary sphincter contraction, pupillary dilation, ejaculation |
| α2 | Adrenergic axon terminals | Inhibit norepinephrine release from adrenergic axon terminals (negative feedback) |
| β1 | Heart, kidneys, adipose tissue | Increase heart rate and force of contraction, increase renin release, increased lipolysis |
| β2 | Smooth muscle in lung, bladder, GI tract, and uterus; pancreas, blood vessels to skeletal muscle | Increased bronchodilation, relaxation of bladder and decreased urination, relaxation of smooth muscle of digestive tract and decreased digestion, relaxation of uterus, increase gluconeogenesis and glycogenolysis, vasodilation and increased blood flow to skeletal muscle |
| β3 | Adipose tissue | Increased lipolysis |
Dual Versus Single Innervation
As we will see, the majority of our organs are dually innervated by both the parasympathetic and sympathetic divisions. Typically, the two divisions have antagonistic effects. For example, the parasympathetic division decreases heart rate and the sympathetic division increases heart rate. However, sometimes they have cooperative effects, like in the external genitalia. The parasympathetic division causes erection of the penis or clitoris, while the sympathetic division causes ejaculation of semen or reflex contraction of the vagina. Although the majority of the organs are dually innervated, some are only innervated by the sympathetic nervous system, such as the sweat glands and blood vessels (Table 7.4).
| Organ | Parasympathetic | Sympathetic |
|---|---|---|
| Adipose tissue | No innervation (no effect) | Increases lipolysis |
| Adrenal medulla | No innervation (no effect) | Stimulates chromaffin cells to release norepinephrine and epinephrine |
| Blood vessels | No innervation except blood vessels to the external genitalia (no effect) | Constricts vessels to visceral organs and skin to divert blood to muscles, brain, and heart |
| Digestive tract organs | Increases motility, increases gastric juice secretion, relaxes sphincters | Decreases motility, decreases gastric juice secretion, constricts sphincters |
| Eyes | Constricts pupils, makes lens bulge for closer vision | Dilates pupils, flattens lens for far vision |
| Gallbladder | Excites | Inhibits |
| Glands (nasal, lacrimal, gastric, pancreas) | Stimulates secretion | Inhibits secretion, constricts blood vessels to glands |
| Hair arrector pili muscles | No innervation (no effect) | Stimulates contraction (goosebumps) |
| Heart (muscle) | Decreases heart rate | Increases heart rate and contractility |
| Heart (coronary blood vessels) | No innervation (no effect) | Vasodilation |
| Kidney | No innervation (no effect) | Promotes renin release |
| Liver | Increases glucose uptake from blood | Increases glucose release into blood |
| Lungs | Constricts bronchioles | Dilates bronchioles |
| Penis | Causes erection | Causes ejaculation |
| Sweat glands | No innervation (no effect) | Stimulates sweating |
| Urinary bladder | Contracts bladder, relaxes sphincter | Relaxes bladder, contracts sphincter |
| Vagina/clitoris | Causes erection of clitoris, increases lubrication | Causes vagina to contract |
Everyday Connections – Fight or Flight? What About Fright and Freeze?
The original usage of the epithet “fight or flight” comes from a scientist named Walter Cannon who worked at Harvard in 1915. The concept of homeostasis and the functioning of the sympathetic system had been introduced in France in the previous century. Cannon expanded the idea and introduced the idea that an animal responds to a threat by preparing to stand and fight or run away. The nature of this response was thoroughly explained in a book on the physiology of pain, hunger, fear, and rage.
When students learn about the sympathetic system and the fight-or-flight response, they often stop and wonder about other responses. If you were faced with a lioness running toward you as pictured at the beginning of this chapter, would you run or would you stand your ground? Some people would say that they would freeze and not know what to do. So isn’t there really more to what the autonomic system does than fight, flight, rest, or digest? What about fear and paralysis in the face of a threat?
The common epithet of “fight or flight” is being enlarged to be “fight, flight, or fright” or even “fight, flight, fright, or freeze.” Cannon’s original contribution was a catchy phrase to express some of what the nervous system does in response to a threat, but it is incomplete. The sympathetic system is responsible for the physiological responses to emotional states. The name “sympathetic” can be said to mean that (“sym-” meaning “together”; “-pathos” meaning “pain,” “suffering,” or “emotion”).
Section Review
The parasympathetic output is based in the brain stem and sacral spinal cord. Neurons from particular nuclei in the brain stem or from the lateral horn of the sacral spinal cord (preganglionic neurons) project to terminal (intramural) ganglia located close to or within the wall of target effectors.
The sympathetic output of the nervous system originates out of the lateral horn of the thoracolumbar spinal cord. An axon from one of these preganglionic neurons projects by way of the ventral spinal nerve root and spinal nerve to a sympathetic ganglion, either in the sympathetic chain ganglia or one of the collateral locations, where it synapses on a postganglionic neuron. The sympathetic system has a specialized preganglionic connection to the adrenal medulla that causes epinephrine and norepinephrine to be released into the bloodstream rather than exciting a neuron that contacts an organ directly. This hormonal component means that the sympathetic chemical signal can spread throughout the body very quickly and affect many organ systems at once.
Review Questions
Critical Thinking Questions
Glossary
adrenal medulla
interior portion of the adrenal (or suprarenal) gland that releases epinephrine and norepinephrine into the bloodstream as hormones
celiac ganglion
one of the collateral ganglia of the sympathetic system that projects to the digestive system
chromaffin cells
neuroendocrine cells of the adrenal medulla that release epinephrine and norepinephrine into the bloodstream as part of sympathetic system activity
ciliary ganglion
one of the terminal ganglia of the parasympathetic system, located in the posterior orbit, axons from which project to the iris
collateral ganglia
ganglia outside of the sympathetic chain that are targets of sympathetic preganglionic fibers, which are the celiac, inferior mesenteric, and superior mesenteric ganglia
craniosacral system
alternate name for the parasympathetic division of the autonomic nervous system that is based on the anatomical location of central neurons in brain stem nuclei and the lateral horn of the sacral spinal cord; also referred to as craniosacral outflow
Edinger–Westphal nucleus
location of parasympathetic neurons that project to the ciliary ganglion
gray rami communicantes
the postganglionic nerve fibers of the sympathetic nervous system
splanchnic nerve
nerve that contains fibers of the preganglionic sympathetic neurons that do not synapse in the chain ganglia
inferior and superior mesenteric ganglion
one of the collateral ganglia of the sympathetic system that projects to the digestive system (there are two)
intramural ganglia
terminal ganglia of the parasympathetic system that are found within the walls of the target effector
paravertebral ganglia
autonomic ganglia superior to the sympathetic chain ganglia
prevertebral ganglia
autonomic ganglia that are anterior to the vertebral column and functionally related to the sympathetic chain ganglia
terminal ganglia
ganglia of the parasympathetic division of the autonomic system, which are located near or within the target effector, the latter also known as intramural ganglia
thoracolumbar system
alternate name for the sympathetic division of the autonomic nervous system that is based on the anatomical location of central neurons in the lateral horn of the thoracic and upper lumbar spinal cord
white rami communicantes
the preganglionic sympathetic outflow from the spinal cord that synapse with the chain (singular ramus communicans)
Glossary Flashcards
This work, Human Physiology, is adapted from Anatomy & Physiology by OpenStax, licensed under CC BY. This edition, with revised content and artwork, is licensed under CC BY-SA except where otherwise noted.
Images from Anatomy & Physiology by OpenStax are licensed under CC BY except where otherwise noted.
Access the original for free at OpenStax.
Image Descriptions
Figure 7.2.1 This anatomical diagram illustrates the autonomic nervous system’s organization in three columns: spinal cord regions (left), associated nerves and terminal ganglia (center), and target organs (right). The left column shows the spinal cord from the brainstem nuclei (Eddinger-Westphal, super salivatory, inferior salivatory, and dorsal nucleus of the vagus) through thoracic (T1-T12), lumbar (L1-L5), and sacral (S1-S5) segments to the coccygeal ganglia. The middle column identifies cranial nerves III, VII, IX, and X with their associated ganglia (ciliary, pterygopalatine, submandibular, and otic). The right column displays target organs including the eye, glands (lacrimal, salivary, adrenal), cardiovascular system (heart, blood vessels), respiratory organs (larynx, trachea, bronchi), digestive organs (esophagus, stomach, liver, pancreas, intestines), and urogenital structures (kidneys, bladder, gonads, external genitalia). Red lines represent sympathetic fibers while blue lines represent parasympathetic fibers, demonstrating how different spinal levels innervate specific organs through the two divisions of the autonomic nervous system. [Return to Figure 7.2.1]
Figure 7.2.2 This diagram illustrates the sympathetic division of the autonomic nervous system organized in three columns: spinal cord regions (left), associated nerves and prevertebral ganglia (center), and target organs (right). The left column displays the spinal cord from the pons and medulla through thoracic (T1-T12), lumbar (L1-L5), and sacral (S1-S5) segments to the coccygeal ganglia, with right and left chain ganglia shown alongside. The middle column identifies key prevertebral ganglia including the superior cervical ganglion, celiac ganglion, greater and lesser splanchnic nerves, superior mesenteric ganglion, and inferior mesenteric ganglion. The right column shows target organs arranged vertically: eye, glands (lacrimal, salivary, parotid, adrenal), cardiovascular structures (heart, abdominal blood vessels), respiratory organs (larynx, trachea, bronchi), digestive organs (esophagus, stomach, liver, pancreas, small and large intestines, rectum), and urogenital structures (kidneys, bladder, gonads, external genitalia). Solid red lines represent preganglionic sympathetic fibers while dashed red lines represent postganglionic sympathetic fibers, demonstrating the two-neuron pathway characteristic of sympathetic innervation from spinal levels to target organs. [Return to Figure 7.2.2]
Figure 7.2.3 This diagram illustrates three distinct organizational patterns of sympathetic nervous system pathways, each shown in two views: a simplified schematic (left) and detailed cross-sectional anatomy (right). Panel (a) demonstrates a central neuron from the T1 spinal level synapsing with a ganglion neuron at the same level within the chain ganglia, with the postganglionic fiber exiting via the white ramus communicans through the spinal nerve to reach target effectors. Panel (b) shows a central neuron from T1 synapsing within a more superior or inferior ganglion in the chain, with multiple branches to different target organs (glands and mucous membranes), where the postganglionic fiber travels via the gray ramus communicans. Panel (c) depicts a central neuron from T5 that projects through the white ramus but bypasses the chain ganglion without synapsing, instead continuing through a splanchnic nerve to synapse within a prevertebral ganglion before reaching target effectors like the stomach. The legend indicates solid red lines represent central neuron axons, dashed red lines represent ganglionic neuron axons, solid red circles mark central neuron cell bodies, hollow red circles mark ganglionic neuron cell bodies, and small circles with lines indicate synapses. [Return to Figure 7.2.3]
Report an Error
Did you find an error, typo, broken link, or other problem in the text? Please follow this link to the error reporting form to submit an error report to the authors.
